 |
.
|
 |
The conservative orthopedic treatment of spondylolisthesis in children is poorly understood. The usual attitude is stopping the sport activity. For degenerative spondylolisthesis in adults, there is little alternative to surgery.
|
 |
|
 |
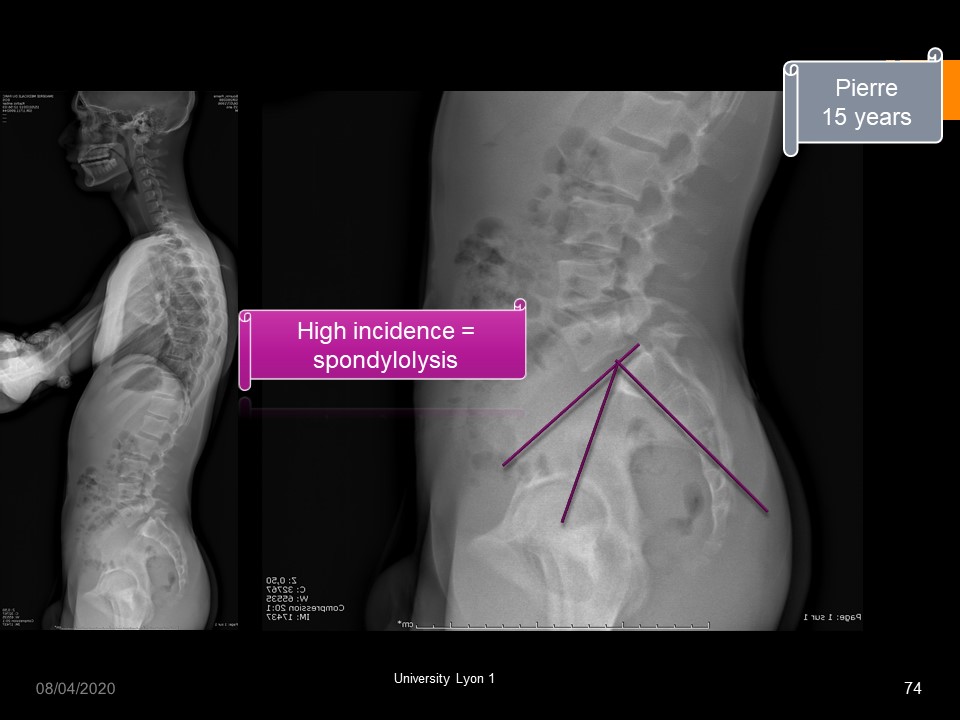
The fracture of the posterior arch of L5 is very frequent among homo sapiens, with however differences according to the origin of the population. It is very common (30 to 60%) among the Inuit who have a specific genetic sequence that allows them to resist at the cold. (Denisov’s man).
|
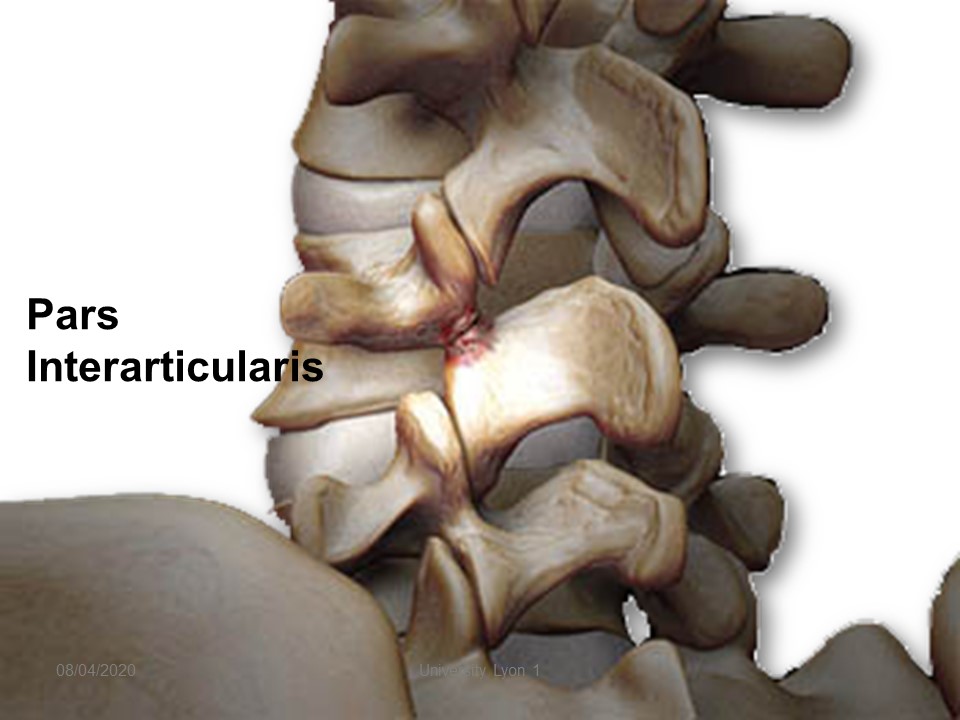 |
The fracture is localized at the level of pars interarticularis between the two facet joints and in front of the lamina.
|
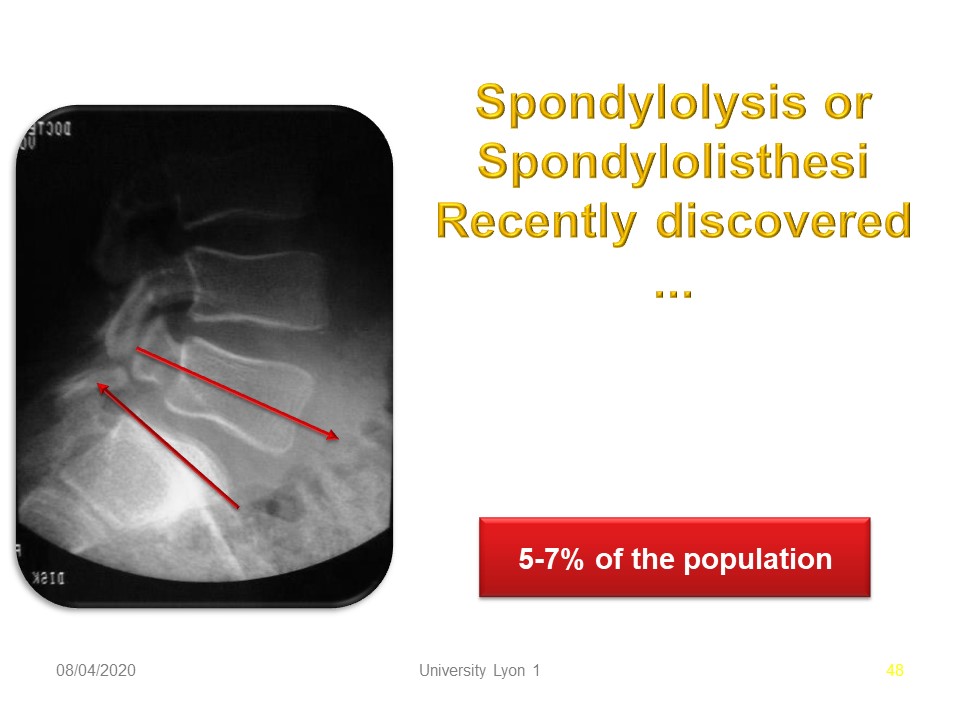 |
The upper facet joint is subjected to forward sliding stress. The lower facet joint is subject to sliding stress up and back. Spondylolysis affects 5 to 7% of the Caucasian population.
|
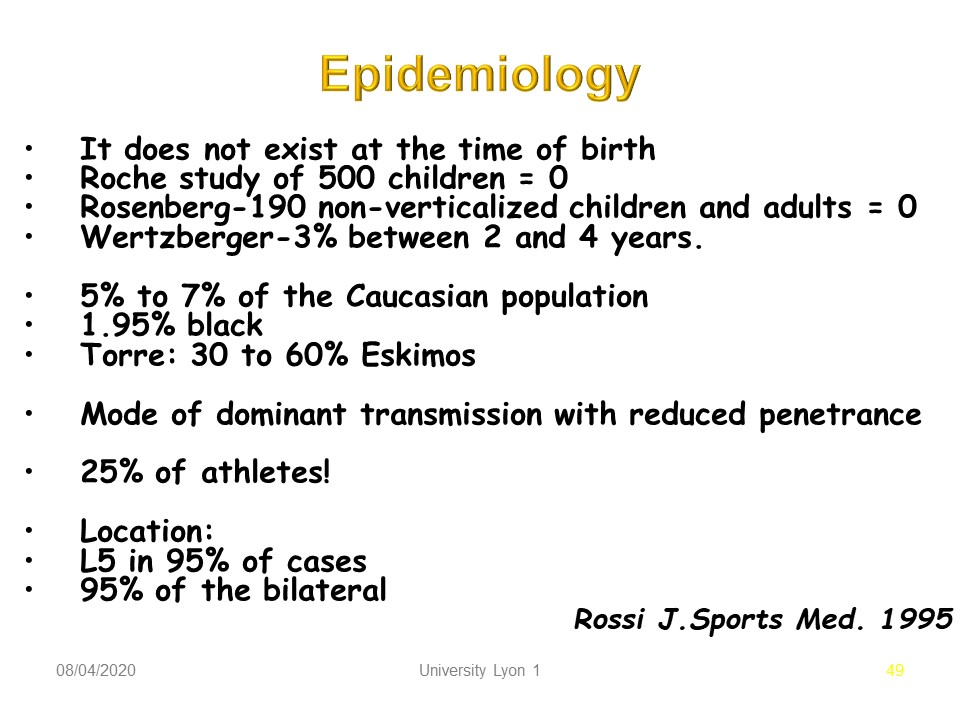 |
The epidemiology was well specified by Rossi in 1995. It does not exist at the time of birth. The mode of transmission is dominant with reduced penetrance. It concerns 25% of athletes. The location is L5 in 95% of cases and bilateral in 95%.
|
 |
Spondylolisthesis is a phenomenon acquired as a result of verticalization. The isthmus is a fuse, but the fracture of fatigue is particular with hereditary predisposition, no pain in most cases, no periosteal callus and spontaneous consolidation. Both forms can be described: Vertical and horizontal sacrum.
|
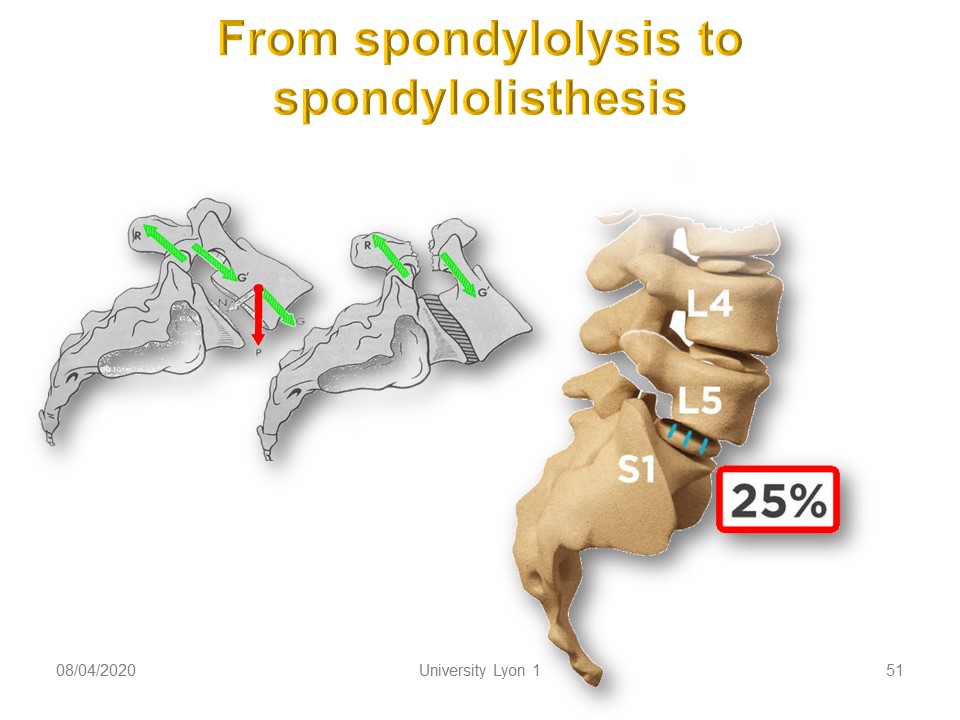 |
Biomechanically, the sliding component increases with the angulation of the sacred slope. Ligament elasticity and sports activity in hyper-extension will promote the gradual slippage in times of growth.
|
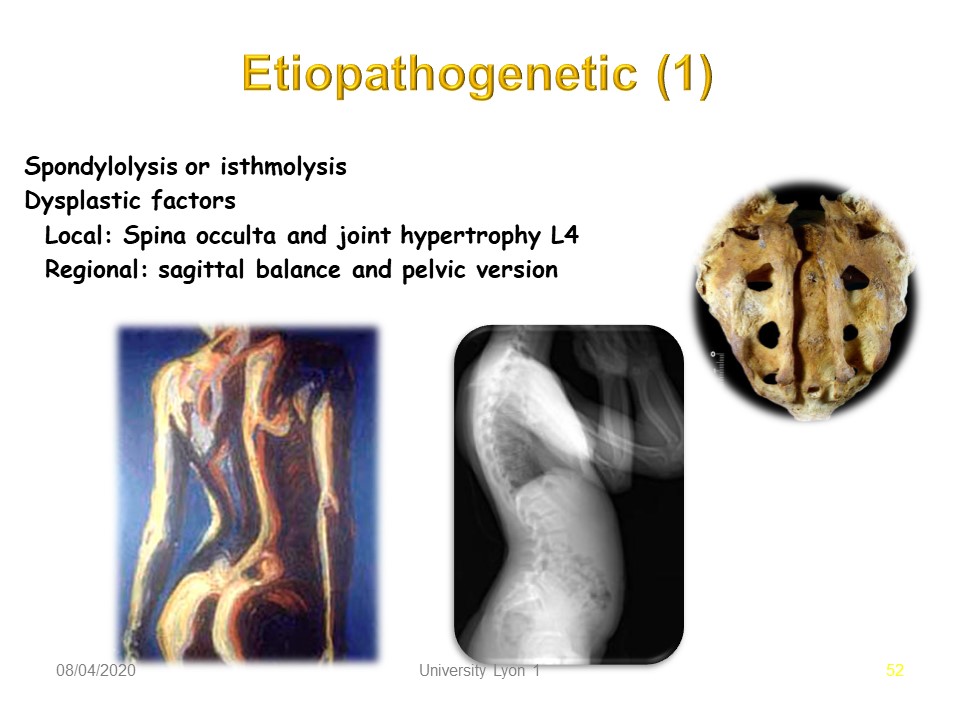 |
Spondylolisthesis does not occur at birth, but bone fragility factors, usually minor forms of spina bifida, promote sliding.
|
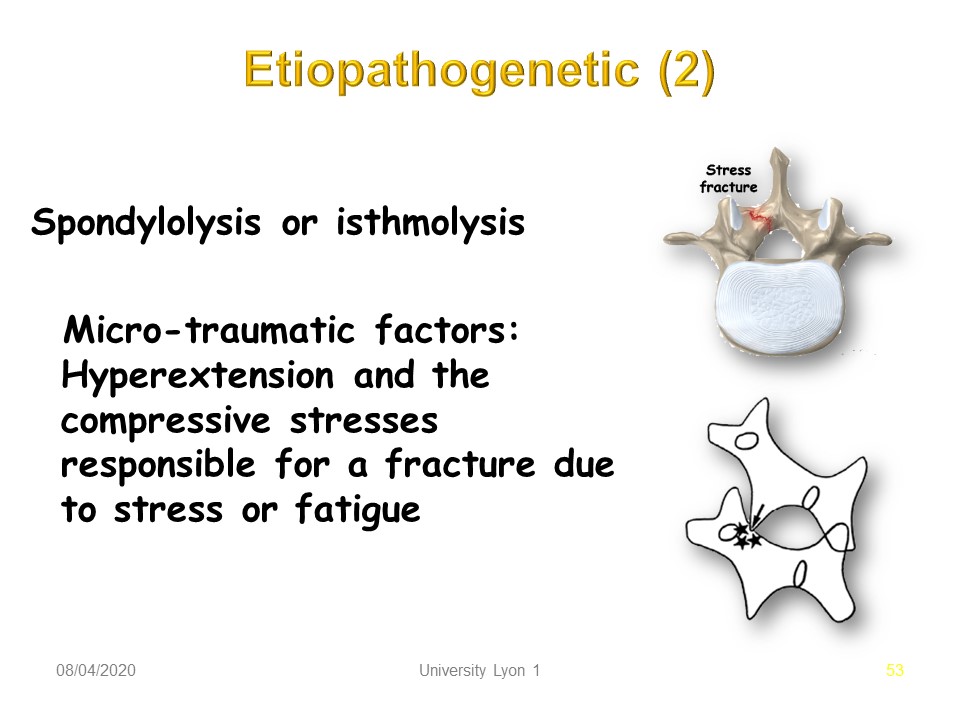 |
Micro-traumatic factors as Hyperextension and the load stress are responsible for the fracture.
|
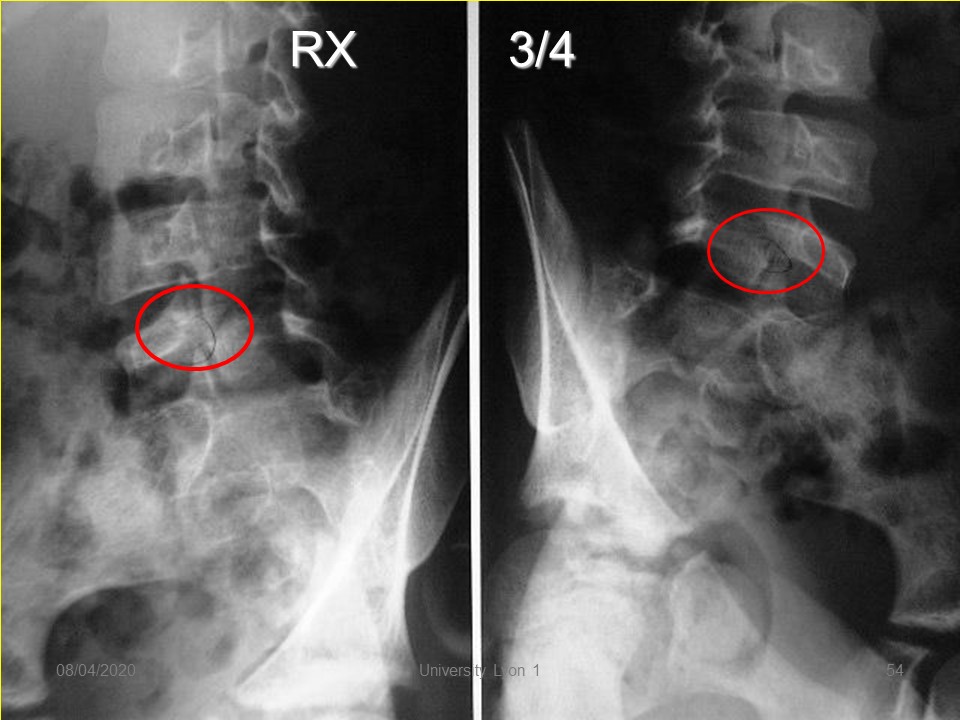 |
Radiologically, the image of ¾ makes it possible to better visualize pars interarticularis when the lysis is of the poorly visible crack type.
|
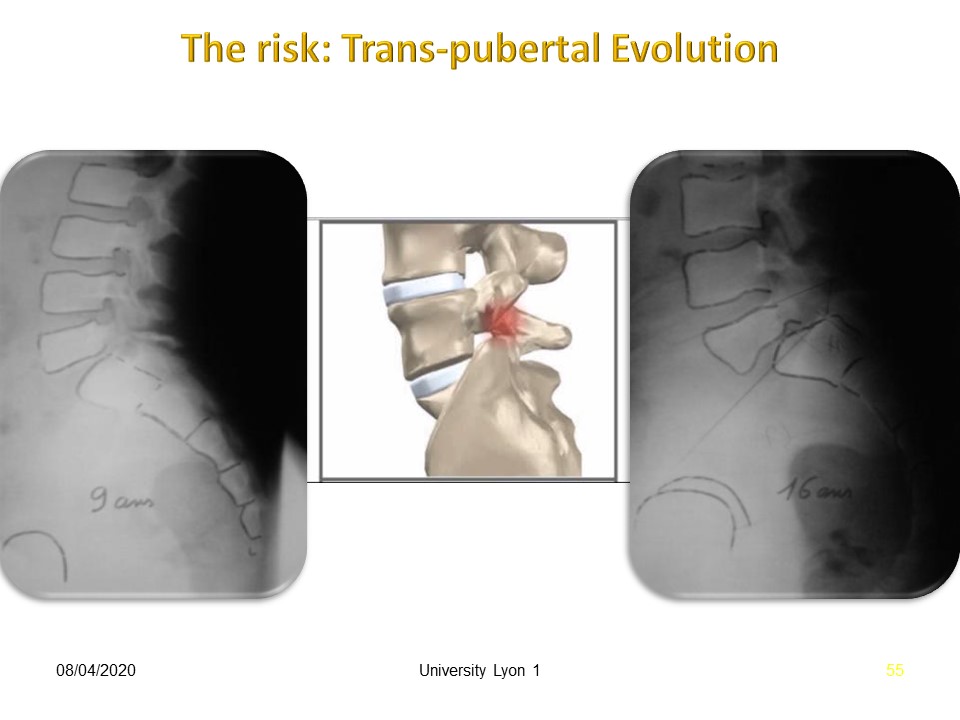 |
Progressive evolution during puberty is classic, despite the cessation of sports activity as in this child, seen at late Risser with significant painful instability.
|
 |
Adult degenerative spondylolisthesis is often associate with Compromised sagittal alignment (compensation): 1. anterior translation of the C7 plumb line. 2. loss of lumbar lordosis. 3. posterior pelvic tilt. The complaints are: 1. Pain: Lumbar and Lower Limb with Possible neurogenic claudication and difficulty with prolonged standing or walking.
|
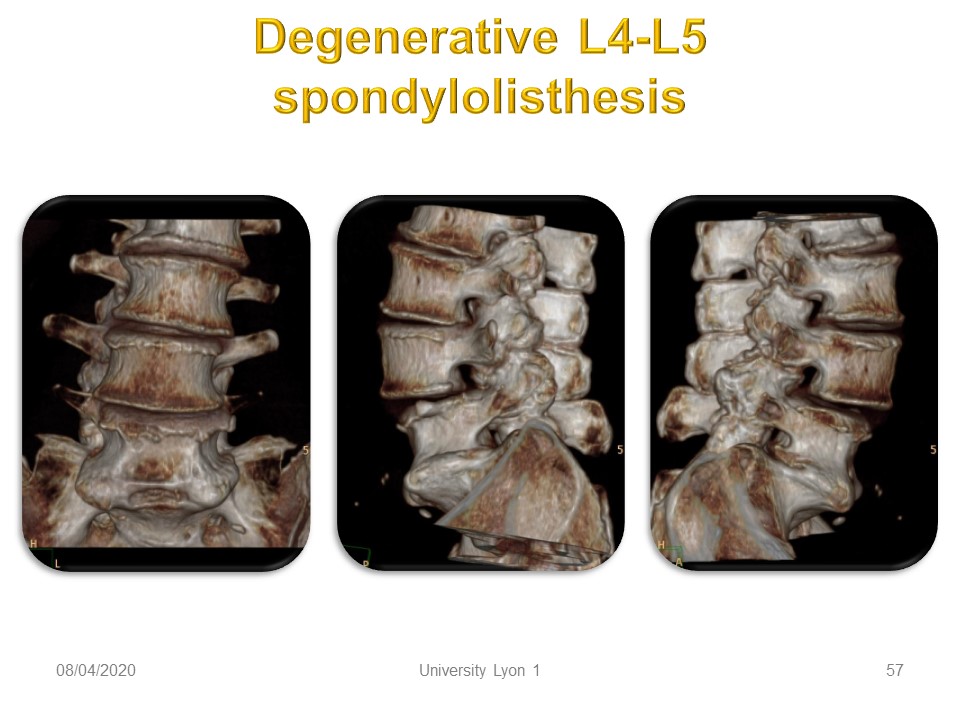 |
Mechanisms are Facet and or disc degeneration. (Jentzsch 2013). Progression is Less likely when disc loses over 80% height or osteophytes present. Progression of symptoms does not correlate with progression of slip.
|
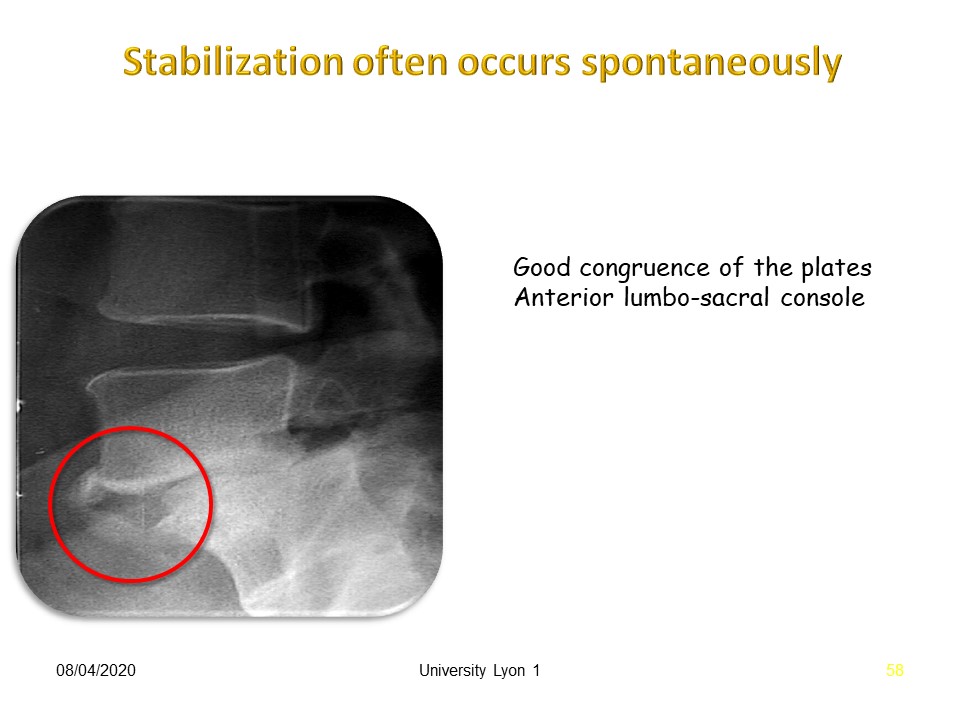 |
Stabilization often occurs spontaneously as in this case with good congruence of the plates and constitution of an Anterior lumbo-sacral console. A video with animation will help to better understand the two types of spondylolisthesis of the child and degenerative in adulthood.
|
 |
The problem is not the diagnosis, but the treatment. Often the sports doctor is wrong regardless of his indications. If he prescribes the sport contra-indication, the consequences are: Weak muscle, weak bone mass and above all, loss of opportunities in sport. If he prescribes to continue the sport activity, the consequences are: progression risk of slippage and responsibility in case of pejorative evolution.
|
 |
.
|
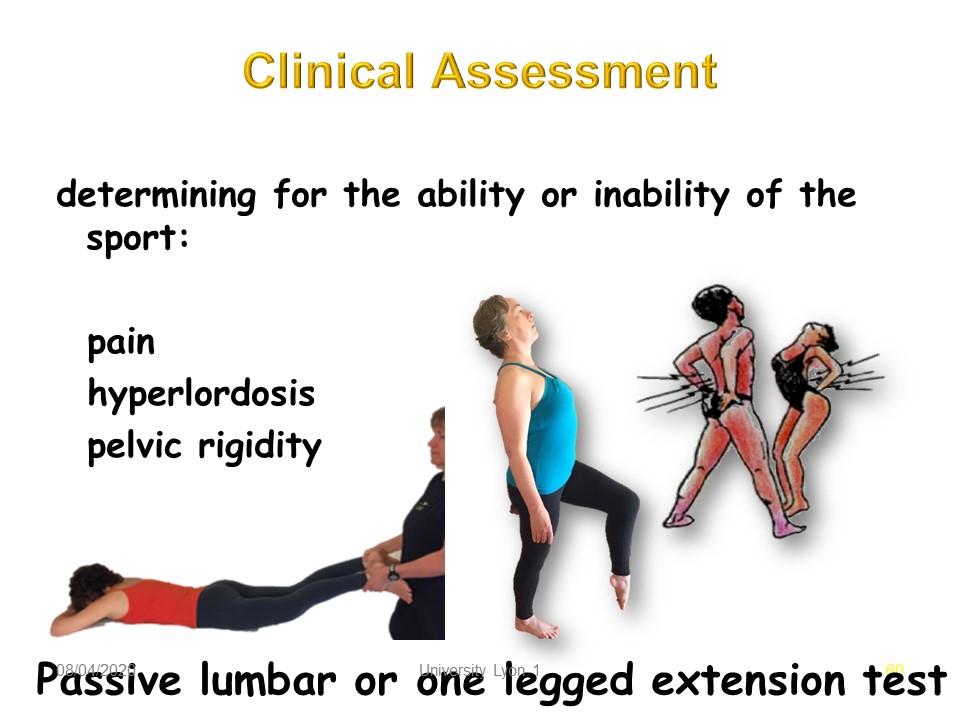 |
To clarify the indications, the clinical examination seeks to find a precise pain by the extension of the lumbar spine in discharge or charge.
|
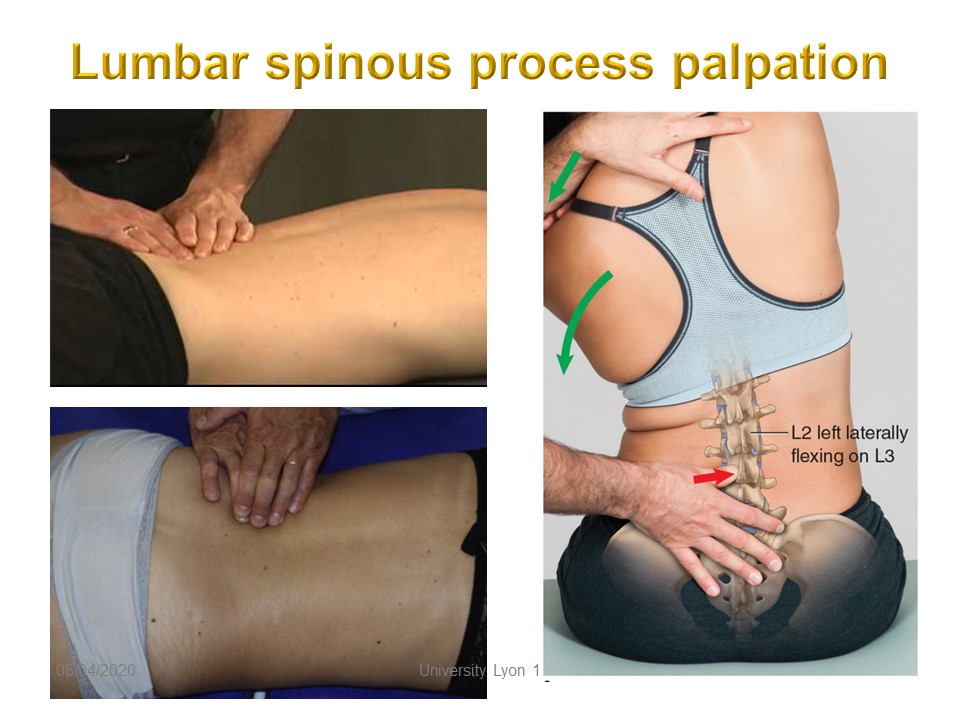 |
But, the most accurate sign is the press pain of an interspinous ligament in the upper left, but especially a press pain of transverse process with both hands resting on each other. The instability test on the right is less specific.
|
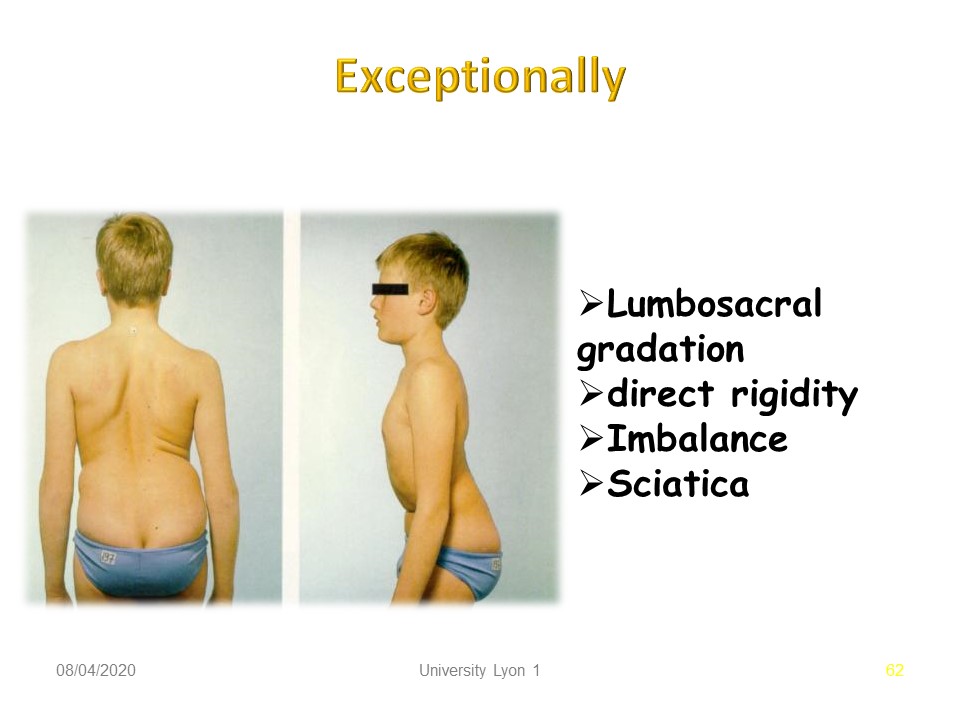 |
Exceptionally, the clinical assessment may reveal an advanced level of slippage such as spondyloptosis. There is a strong rigidity in the sagittal plane, a frontal and sagittal joint imbalance with hip flexed to rebalance the spine. During adolescence this evolution can be rapid and there are often signs of sciatica.
|
 |
|
 |
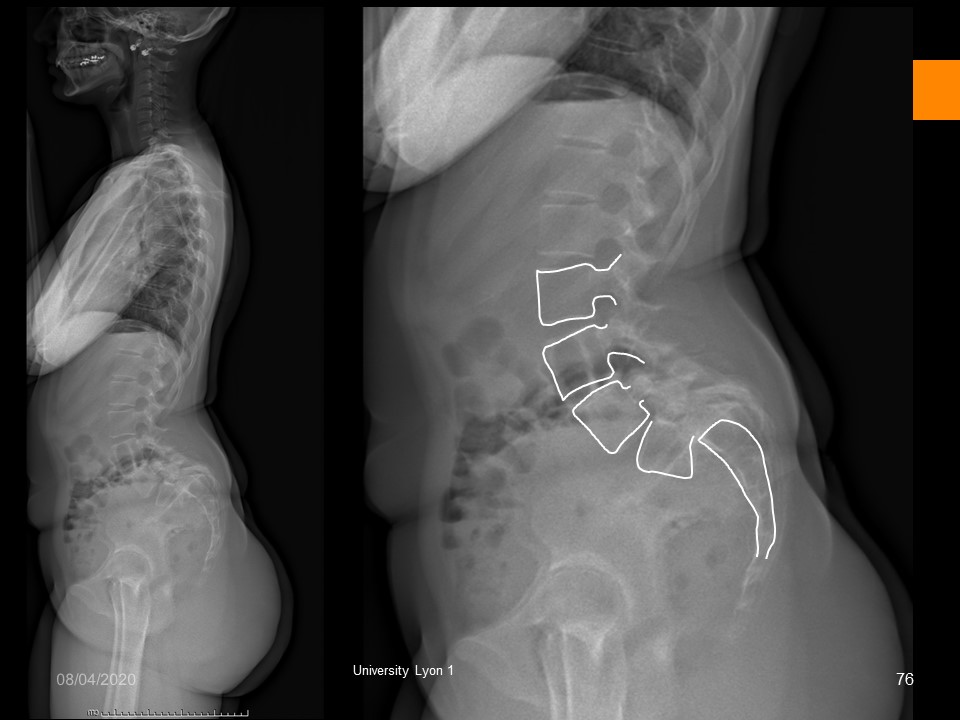
The radiological assessment is always necessary to determine the ability or inability of the Sport. We will measure: 1, the lumbo-pelvic incidence and the lumbo-sacral angle. 2. The verticalization of the sacrum. 3. The L5 deformation (old or new). 3. The Sliding gradation of Meyerding. 4. The Cobb angle of the possible scoliosis associated.
|
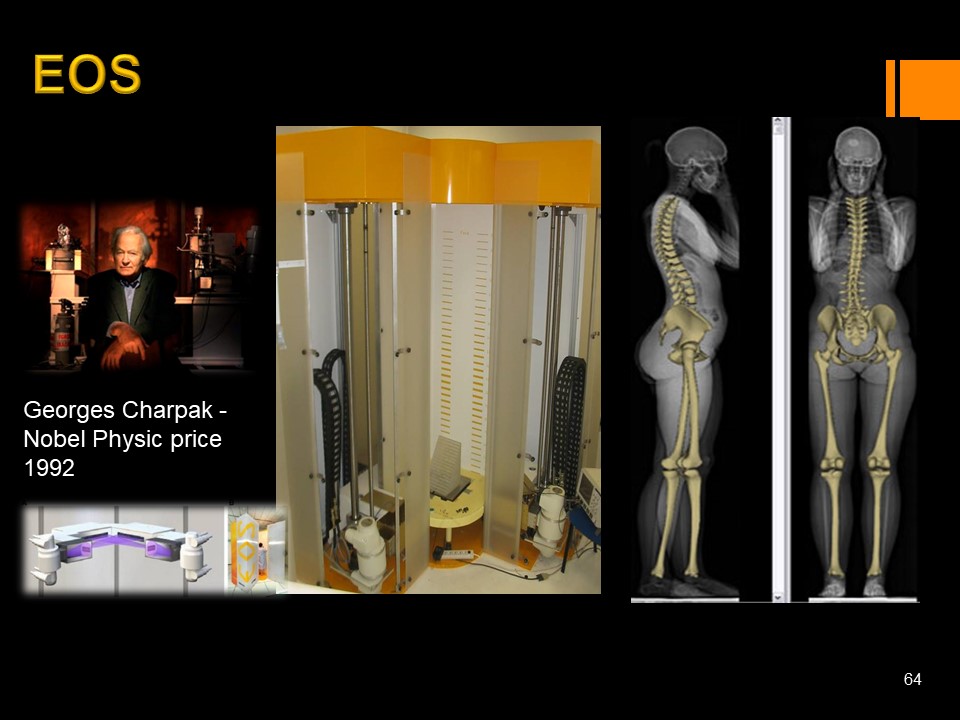 |
EOS radiology automatically measures most lumbo-pelvic parameters, which are essential for spondylolisthesis. Remember that in ultra-low dose, irradiation is 25 times lower than conventional irradiation.
|
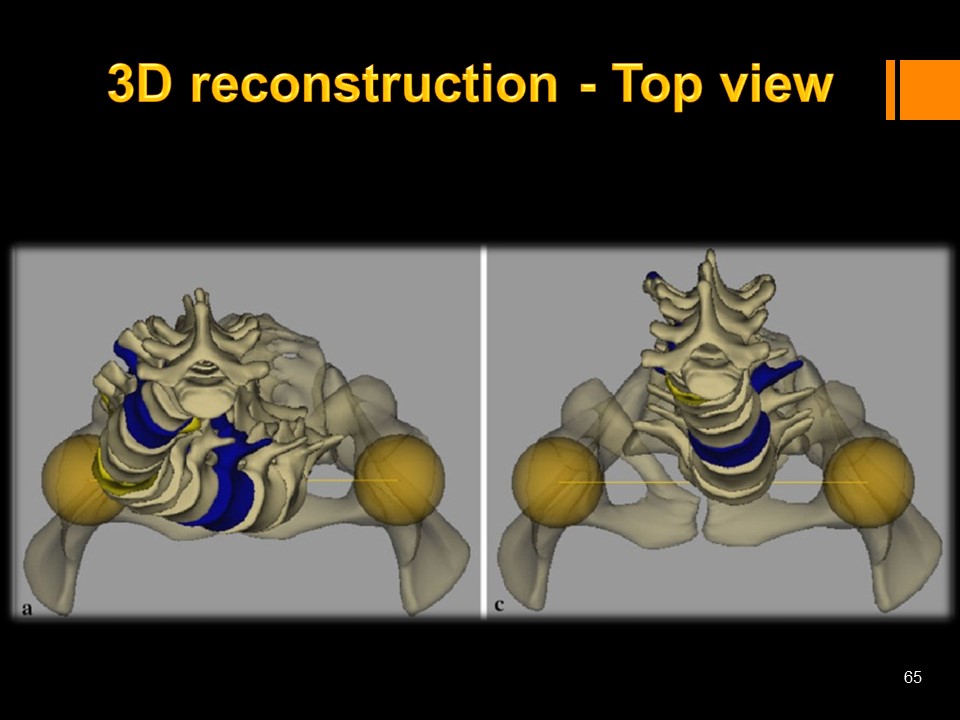 |
The view from above or da Vinci view, allows to better appreciate the imbalances.
|
 |
The lumbo-pelvic parameters and in particular, the lumbo-pelvic incidence were described by Mrs. Duval Beaupère. They are useful in both children and adults. Lumbo-pelvic incidence has the advantage of being a constitutional factor that does not vary between 7 and 45 years. It can, however, evolve in adults with pelvic retroversion. The lumbosacral incidence is the sum of the sacral base angler and the pelvic version. There is also a very good correlation with lumbar lordosis.
|
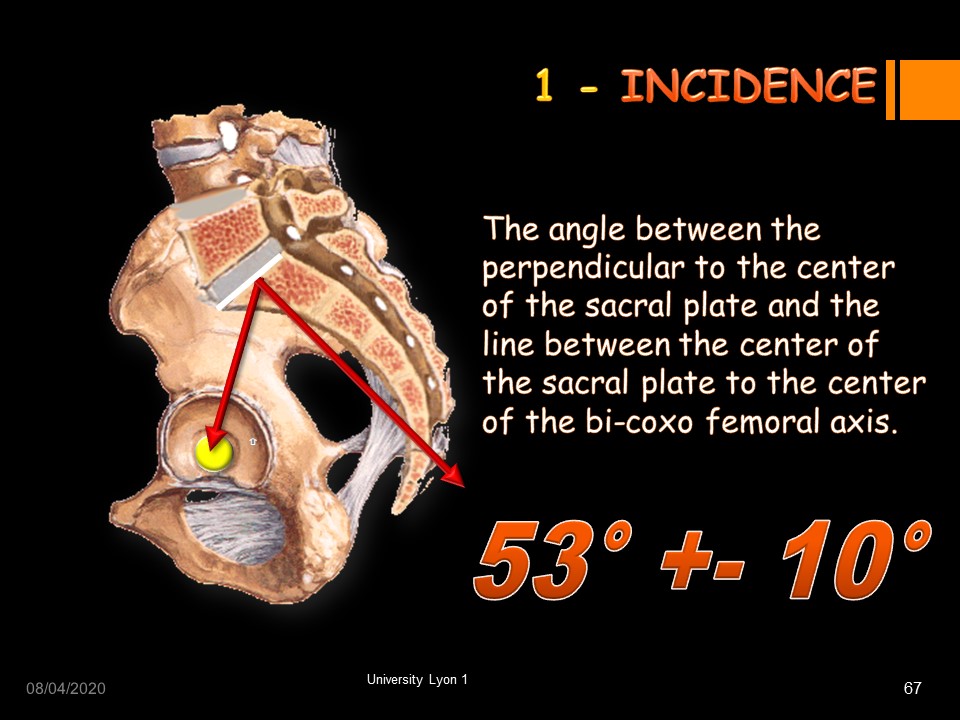 |
The lumbo-pelvic incidence is the angle between the perpendicular to the center of the first sacral plate and the line between the center of the sacral plate to the center of the bi-coxo femoral axis. The average angulation is 53 ° (standard deviation 10 °).
|
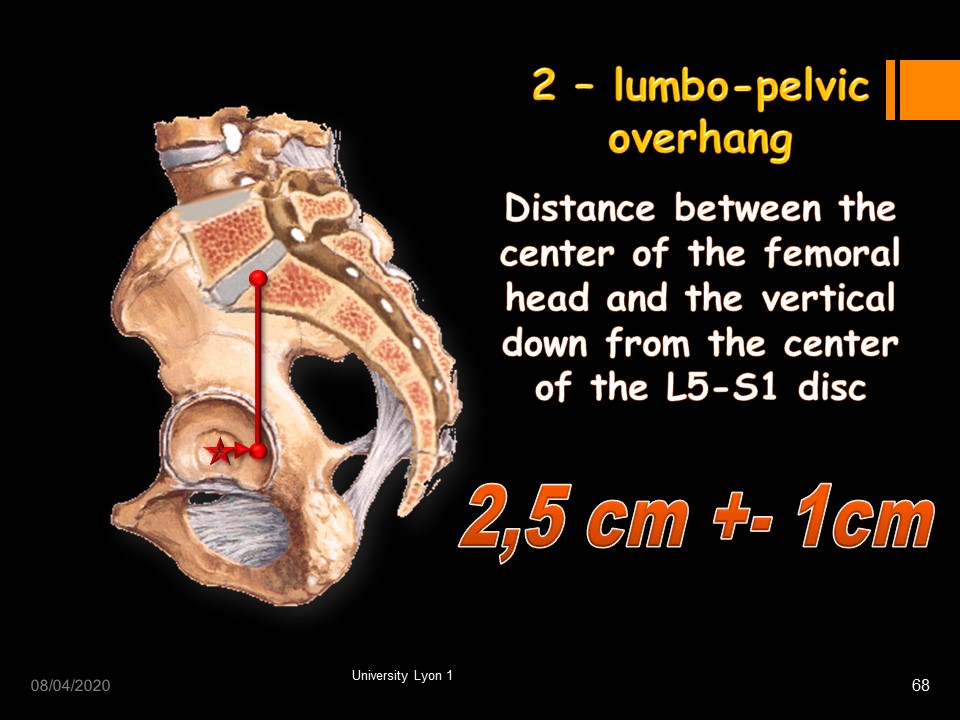 |
The lumbo-pelvic overhang is the Distance between the center of the femoral head and the vertical down from the middle of the upper S1 plate. The average distance is 2.5 cm (standard deviation 1 cm).
|
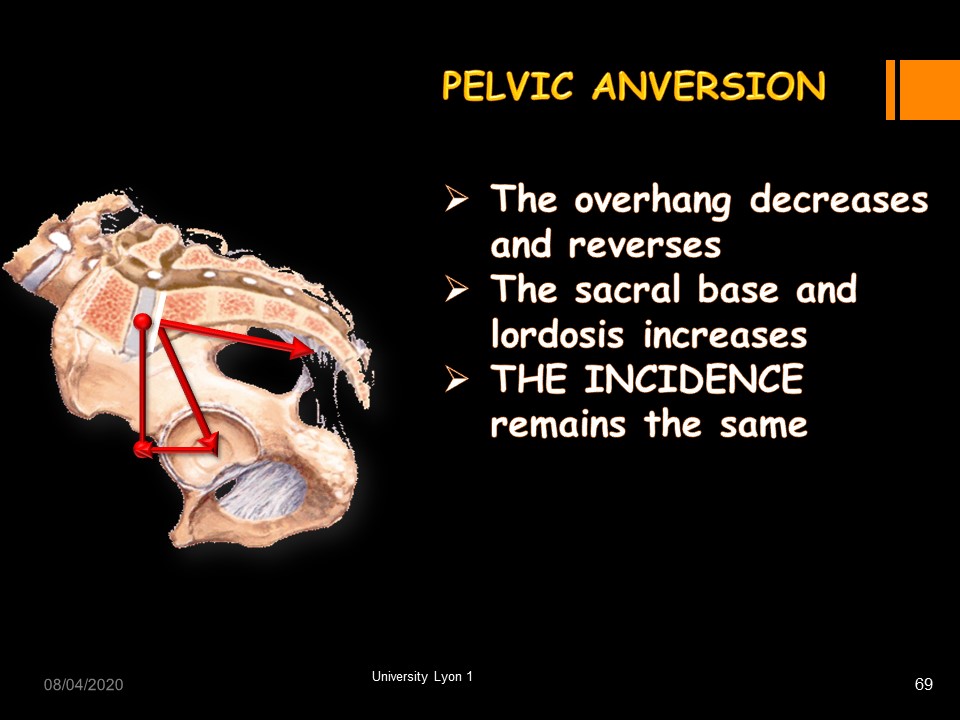 |
In pelvic anteversion, the overhang decreases and reverses, the sacral base and lordosis increases, THE INCIDENCE remains the same.
|
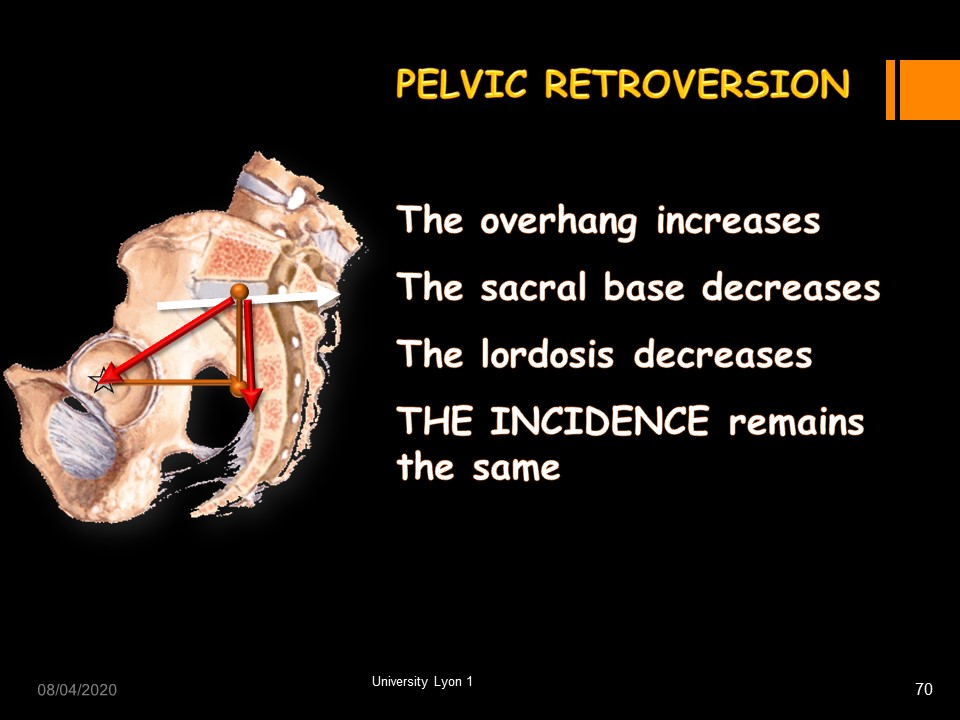 |
In pelvic retroversion, The overhang increases. The sacral base decreases. The lordosis decreases. THE INCIDENCE remains the same.
|
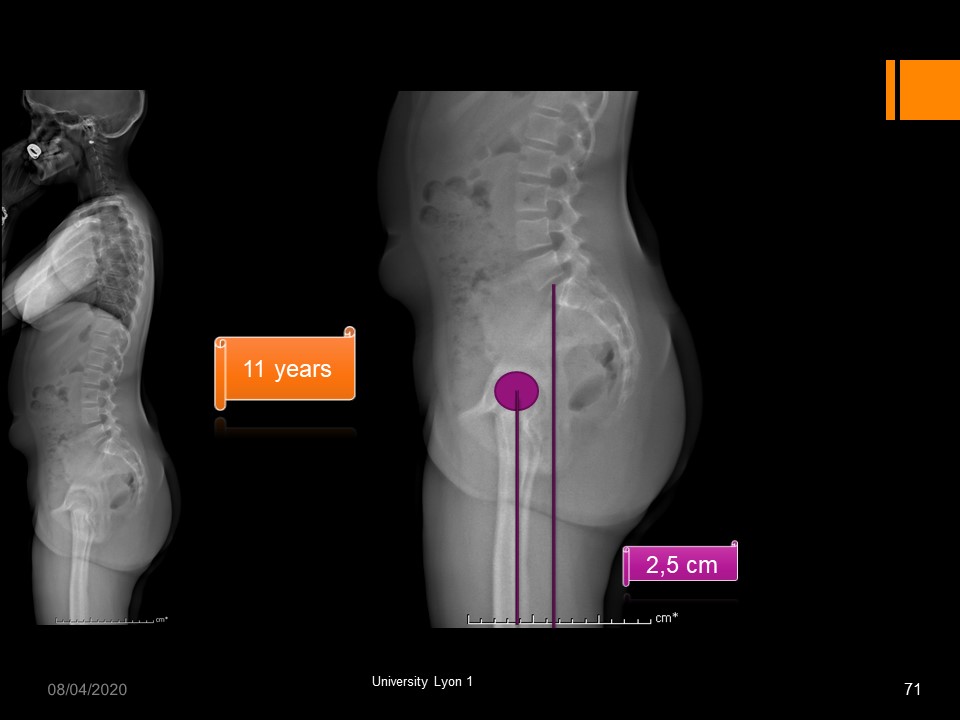 |
This patient has a well-balanced physiological morphostatic.
|
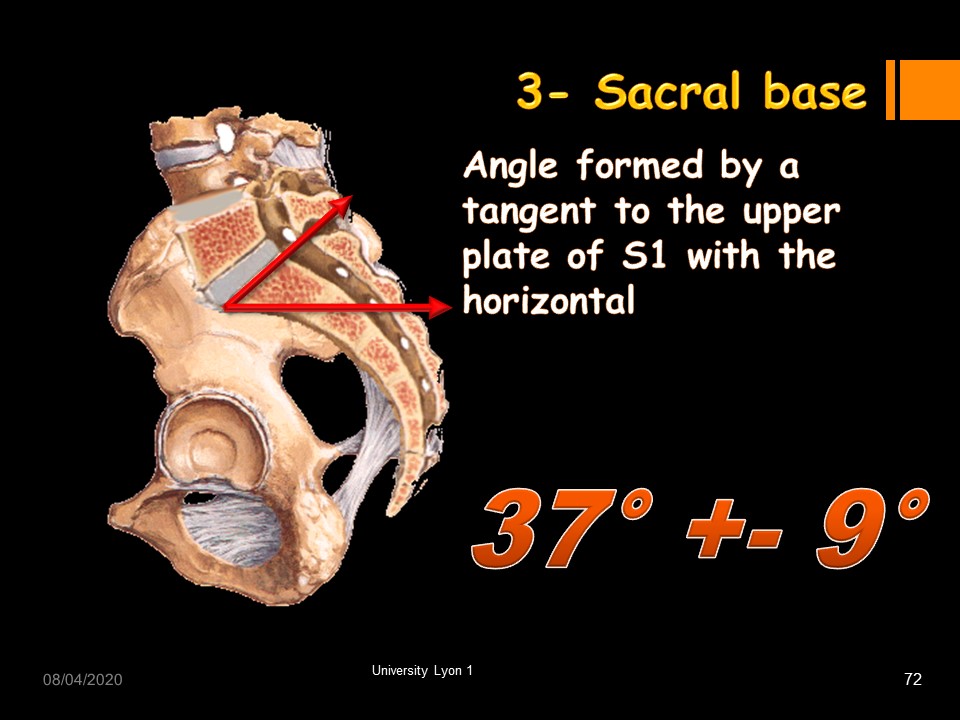 |
The sacral base angle is the Angle formed by a tangent to the upper plate of S1 with the horizontal. We have seen that the slippage component increases with this angle.
|
 |
Several morphotypes are classic. For example, thoraco-lumbar kyphosis associated with low incidence.
|
 |
Spondylolysis with high incidence. In this case hyperkyphosis is associated.
|
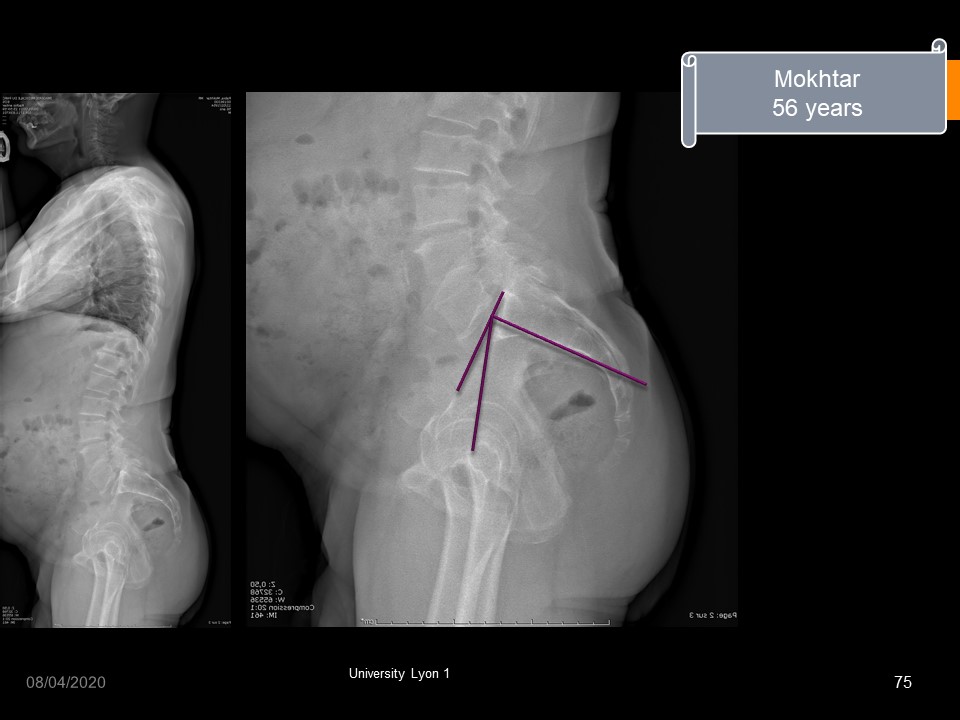 |
Despite a high lumbo-pelvic incidence, this adult patient has minimal slippage, but there is significant posterior facet joints arthrosis.
|
 |
This patient presents a beginning of spondyloptosis with verticalization of the sacrum and strong increase of the overhang. The prognosis is unfavorable, and the surgery must be discussed.
|
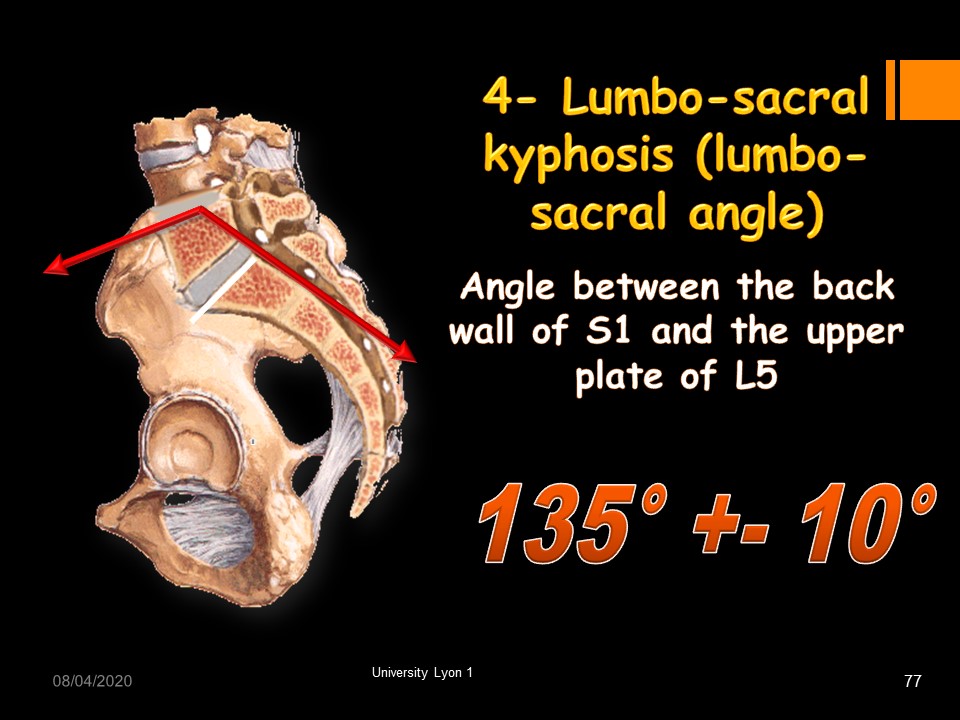 |
Due to the deformation of the vertebral body of L5, another angle specific to spondylolisthesis has been described: the lumbosacral angle. It corresponds to lumbosacral kyphosis. It is the Angle between a tangent to the back wall of S1 and a tangent to the upper plate of L5. The average angulation is 135 ° (standard deviation 10 °).
|
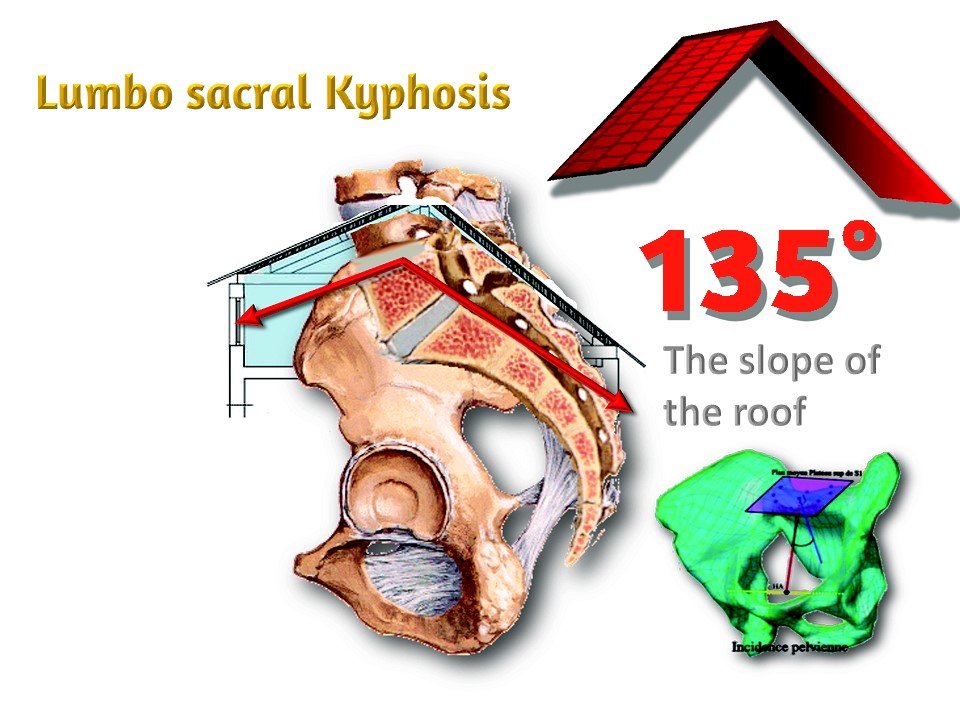 |
This angle integrates the deformation of the vertebral body of L5 and the verticalization of the sacrum. It corresponds somewhat to the slope of a roof. If the angle decreases, the slope of the roof increases. Below 110 °, a brace is needed in children. Below 90 °, surgery is discussed.
|
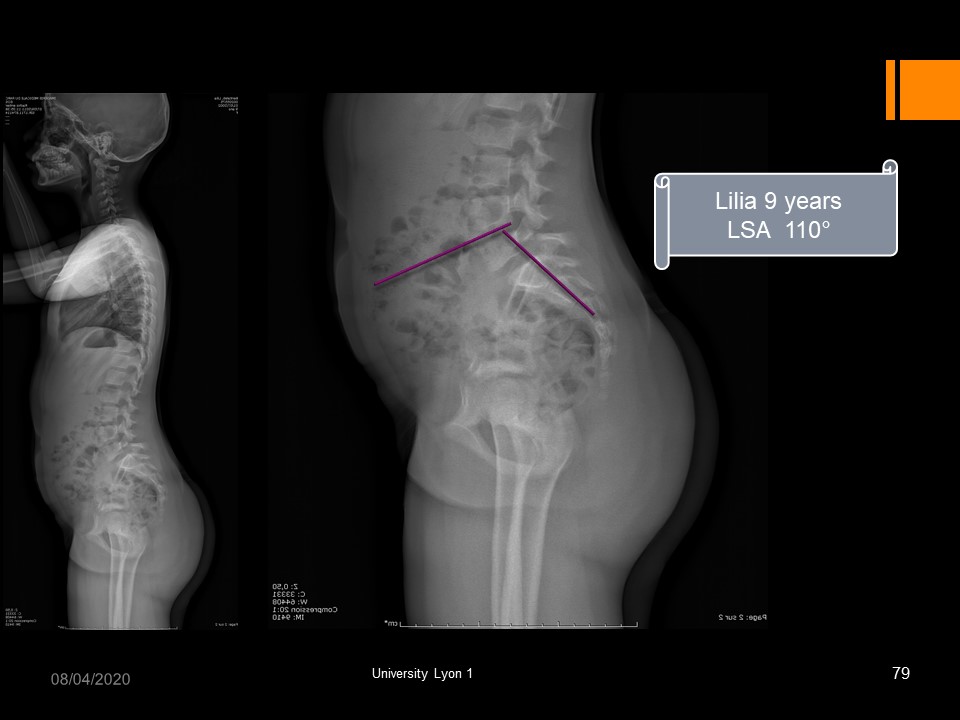 |
In this 9-year-old girl with L5 spondylolysis, the lumbosacral angle is 110 °. The evolutionary prognosis is important, and a brace is discussed according to the sports activity.
|
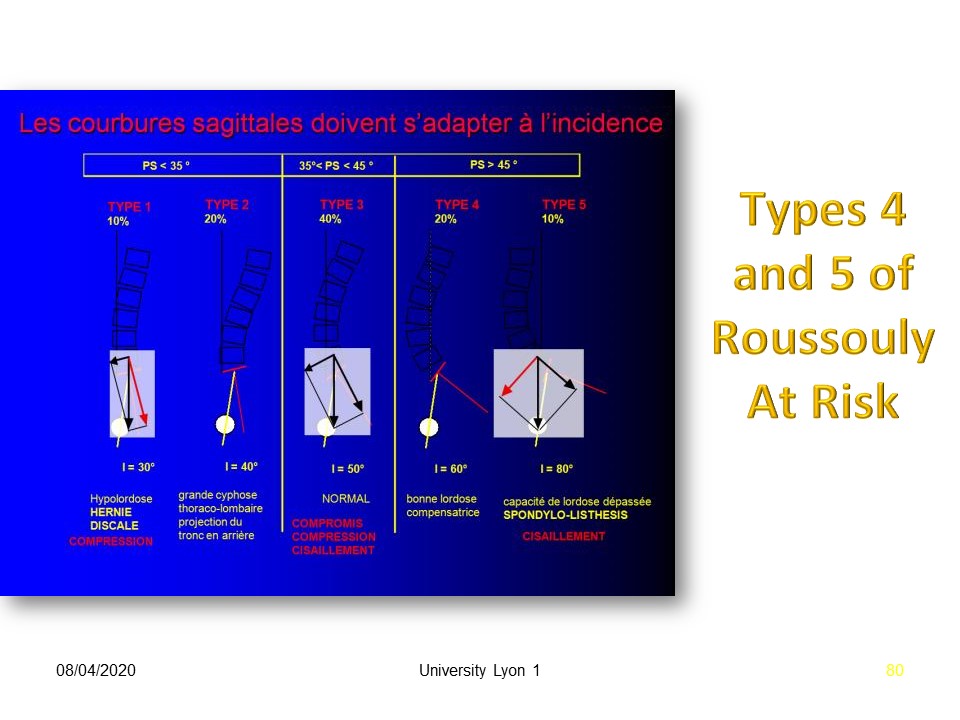 |
Roussouly described the adaptation of the spine to different incidences. Types 4 and 5 are at risk for spondylolisthesis.
|
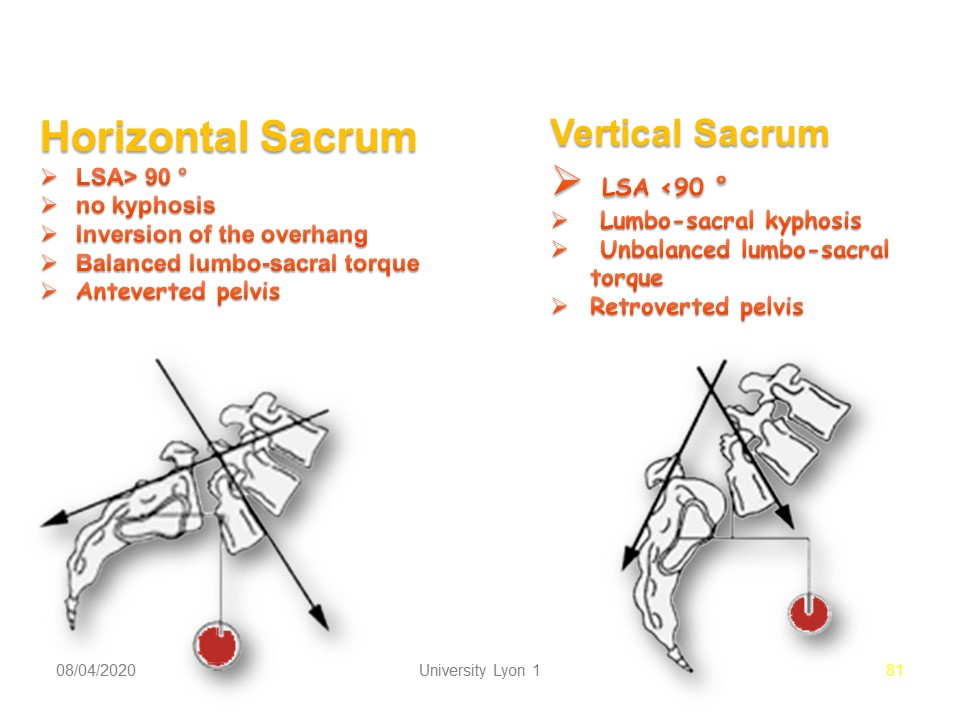 |
The verticalization of the sacrum is an important parameter, especially since poorly made braces can accentuate verticalization. The characteristics of the vertical sacrum are: Lumbo-sacral angle > 90 °. no lumbo-sacral kyphosis. Inversion of the overhang, Balanced lumbo-sacral torque. Anteverted pelvis. The characteristics of the horizontal sacrum are: Lumbo-sacral angle
|
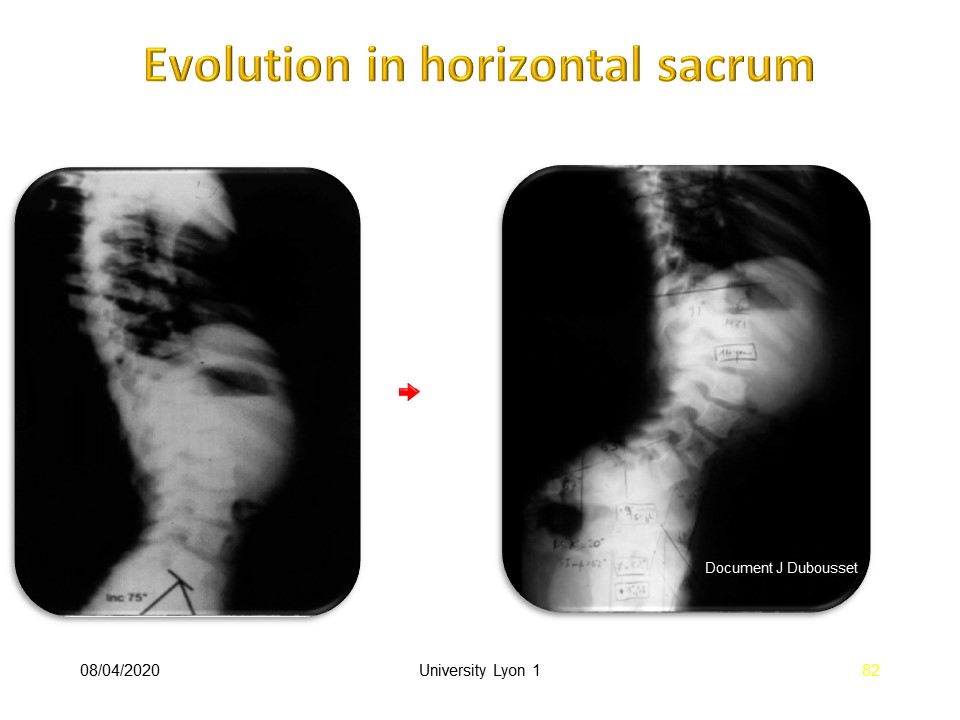 |
In this neurological patient, favorable evolution with horizontal sacrum, despite a total lordosis of the trunk.
|
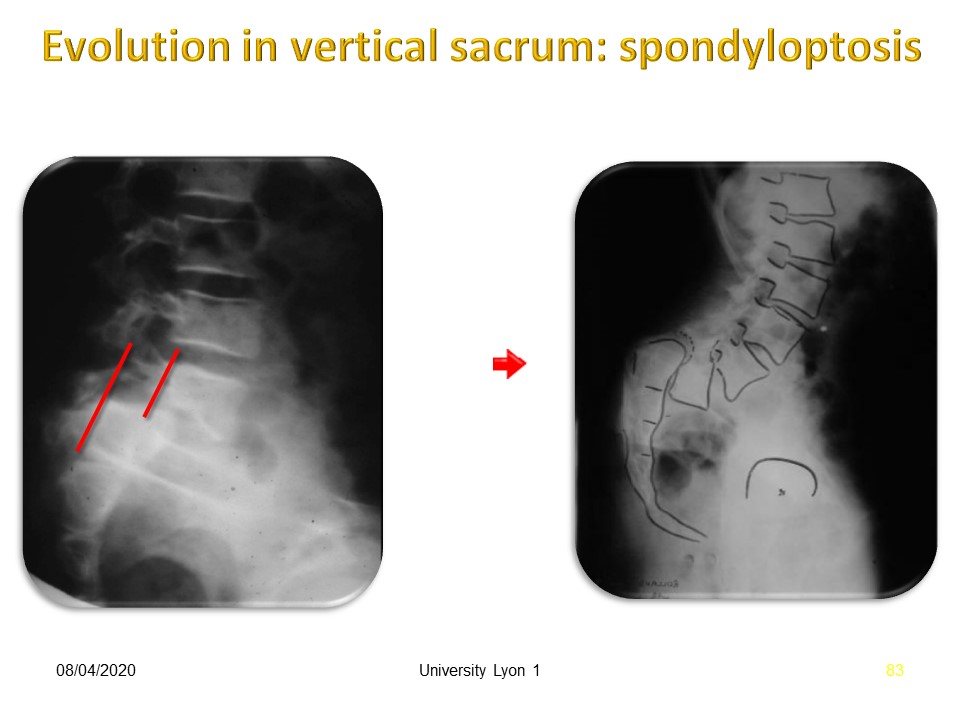 |
On the left the slippage is a stage III, but especially the sacrum is verticalized and the risk of evolution towards the spondyloptosis is major.
|
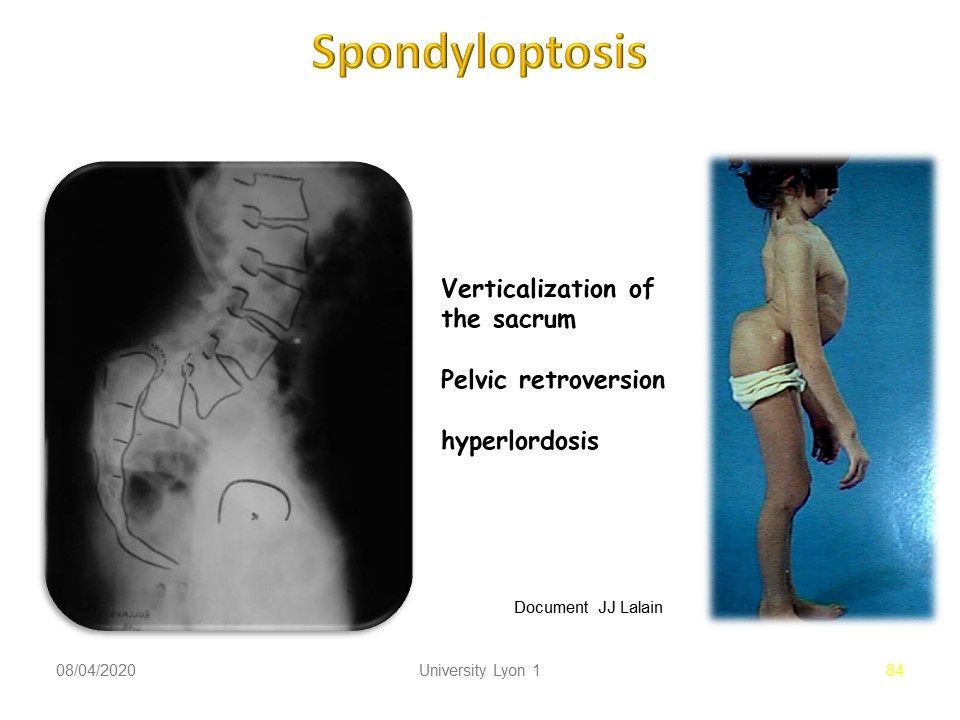 |
In this patient, Spondyloptosis is typical with vertical sacrum, pelvic retroversion and total hyperlordosis of compensation.
|
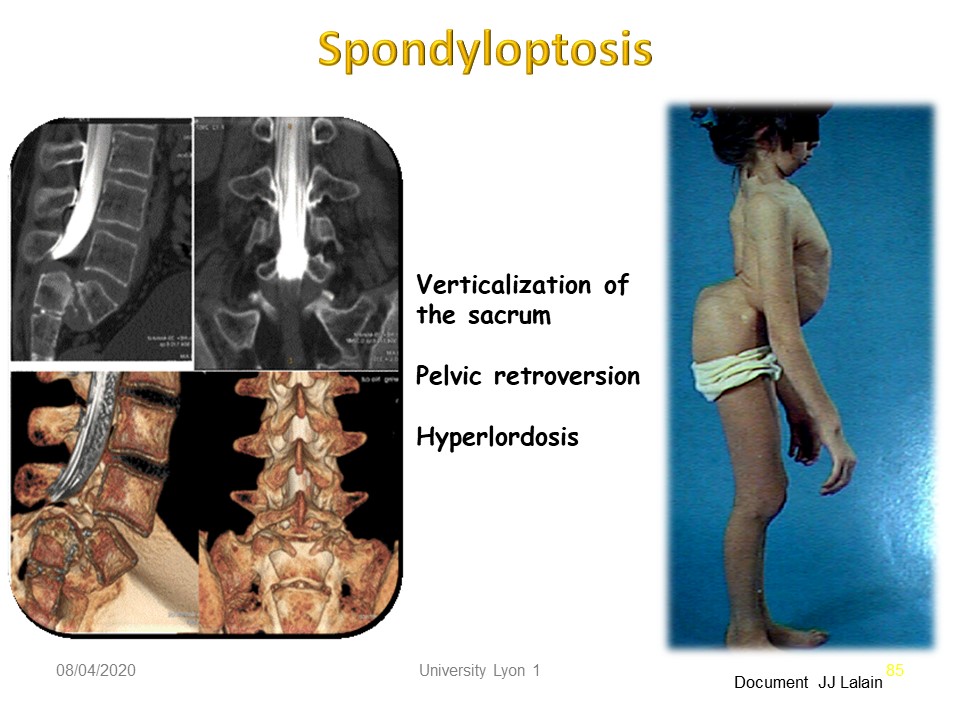 |
3D reconstruction shows the stretching of the L5 spine that can be tolerated for many years if evolution is slow.
|
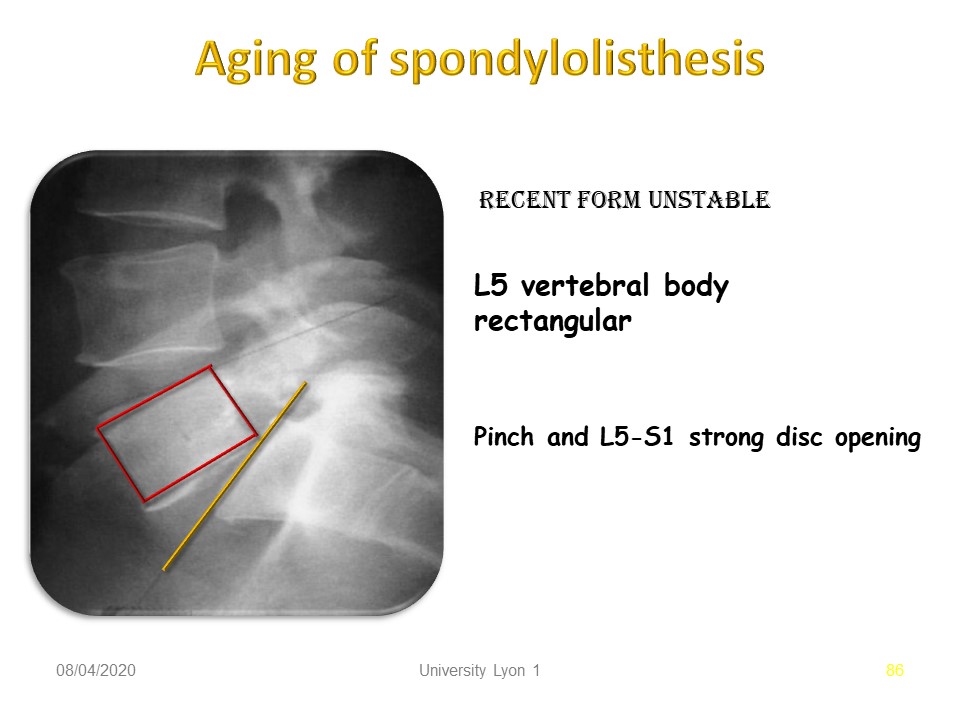 |
The age of spondylolisthesis and the assessment of the quality of the L5 - S1 disc are criteria that point towards conservative orthopedic treatment. Here low deformity of the vertebral body of L5 corresponding to a recent lysis, may be a consequence of discopathy. Pinching and strong opening of the L5-S1 disc confirm the painful instability.
|
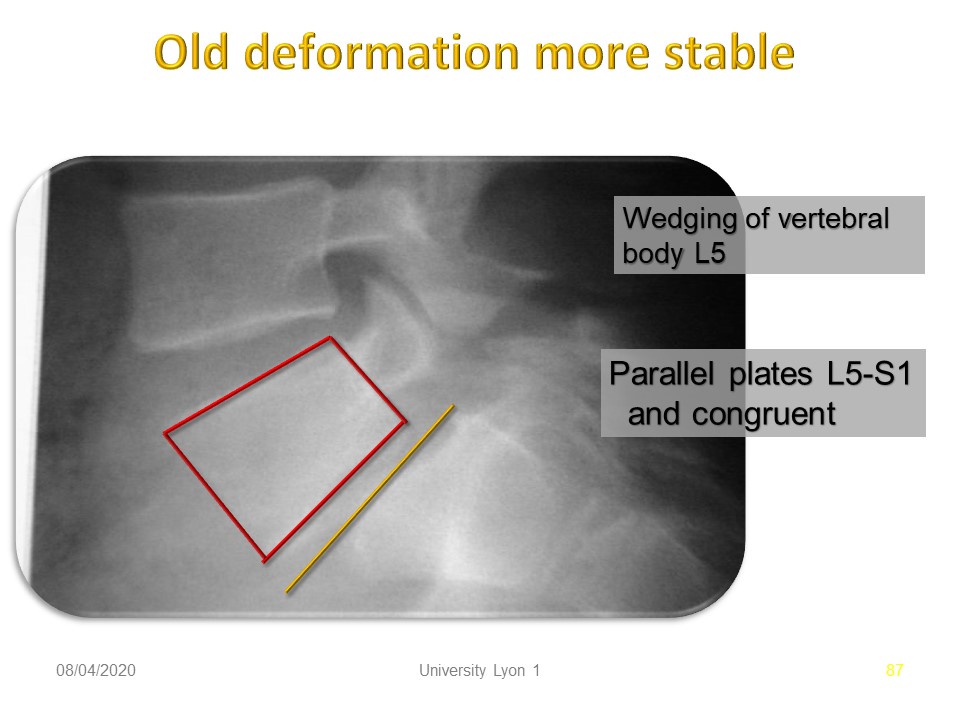 |
The wedging of L5 reflects the age of the slip. The congruence of the trays and the low opening of the L5-S1 disc reflect the good adaptation of the disc.
|
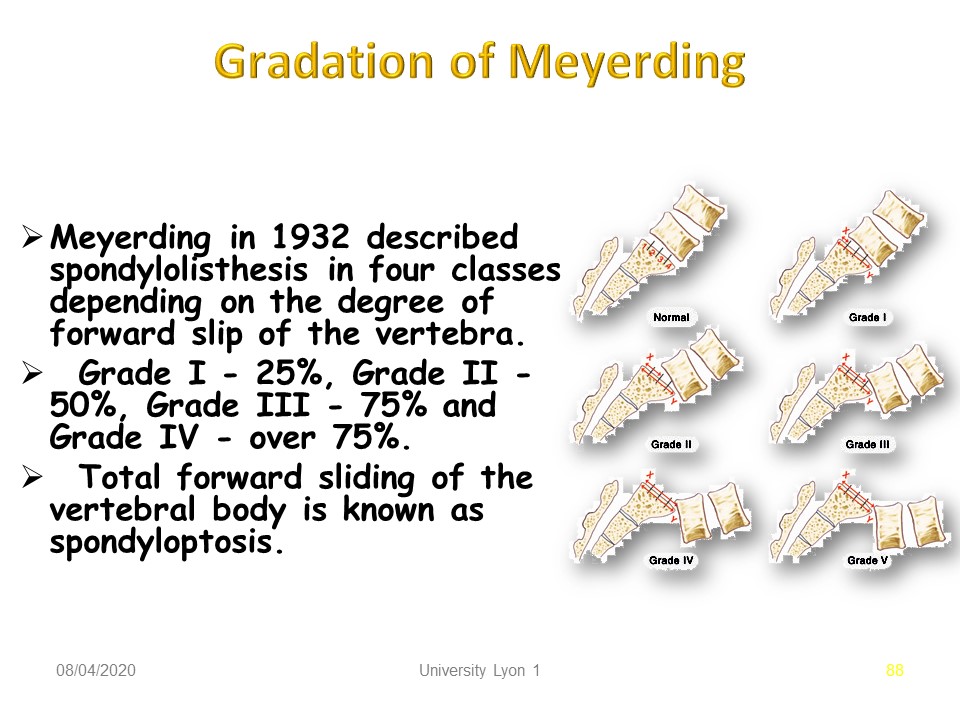 |
Meyerding in 1932 described spondylolisthesis in four classes depending on the degree of forward slip of the vertebra. Grade I - 25%. Grade II - 50%. Grade III - 75% and, Grade IV - over 75%. Total forward sliding of the vertebral body is known as spondyloptosis.
|
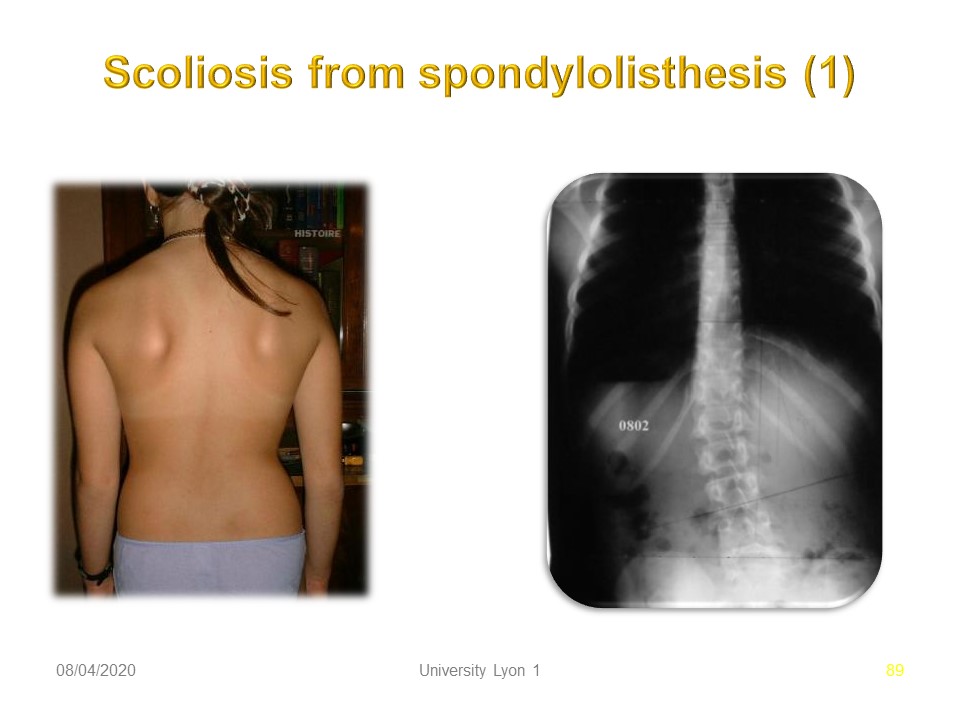 |
In 20% of cases, lumbar scoliosis is associated with spondylolisthesis. The radiological evolution has been well described by Maldague with initially unilateral left sliding, compensation by left lumbar scoliotic attitude which little by little is going to be structuralized. Then bilateralization of the sliding on the side of the concavity.
|
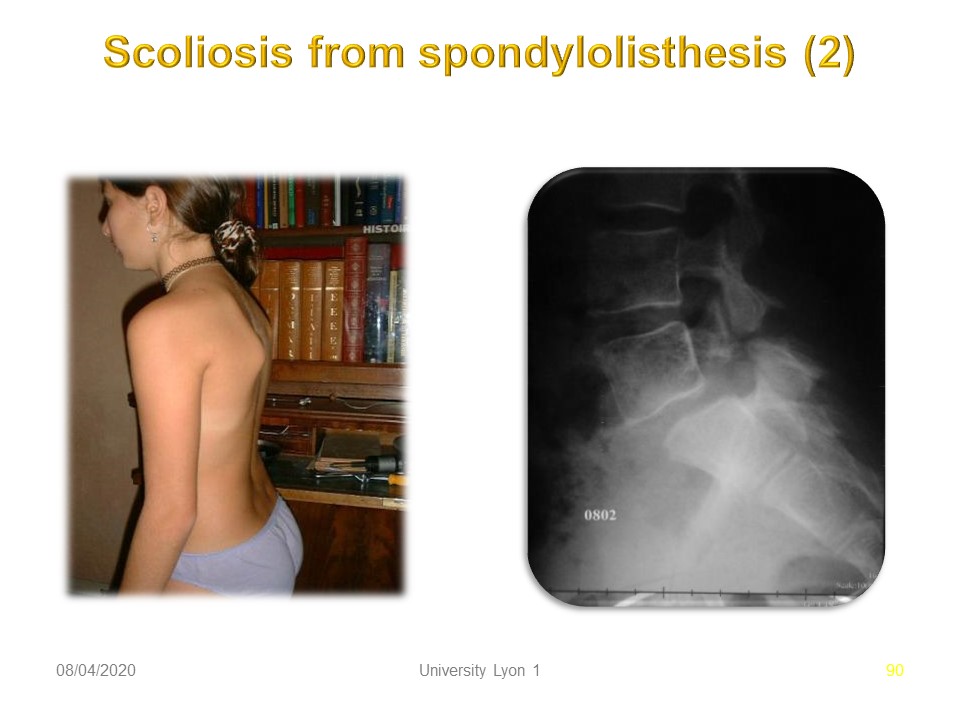 |
In this child, we note a projection of the trunk forward, probably by antalgic attitude.
|
 |
Many other imaging exams can be done. They are used in special cases and should not be systematic. These are: X-ray, Dynamic X-ray, CT scan, 3D reconstruction, RMI, Scintigraphy.
|
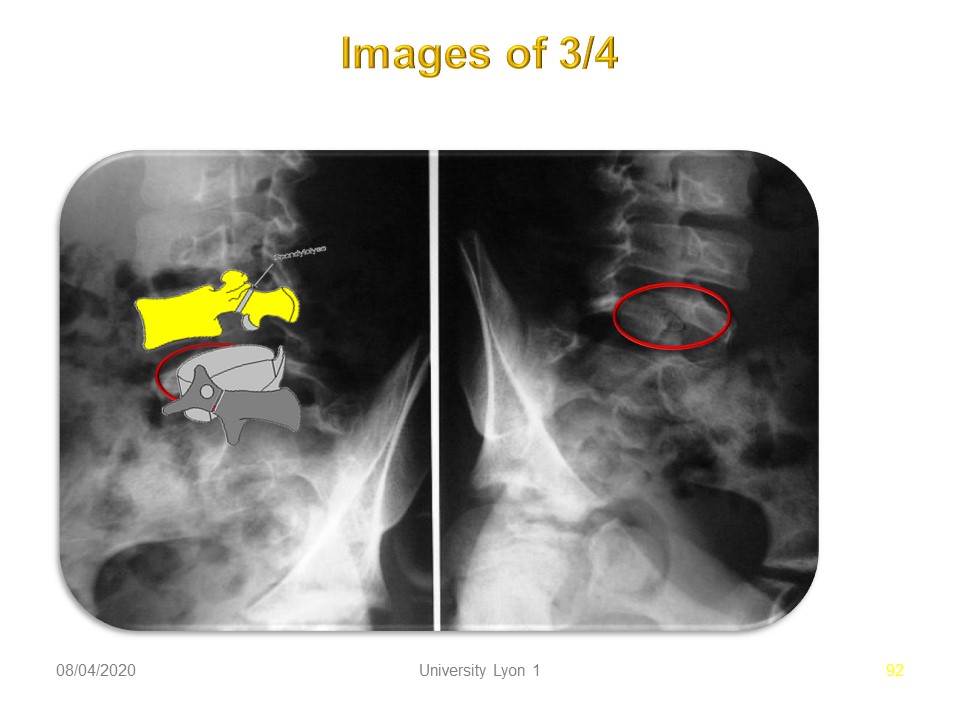 |
The radiography of ¾ makes it possible to better visualize the pars interarticularis when the lysis is of crack type poorly visible.
|
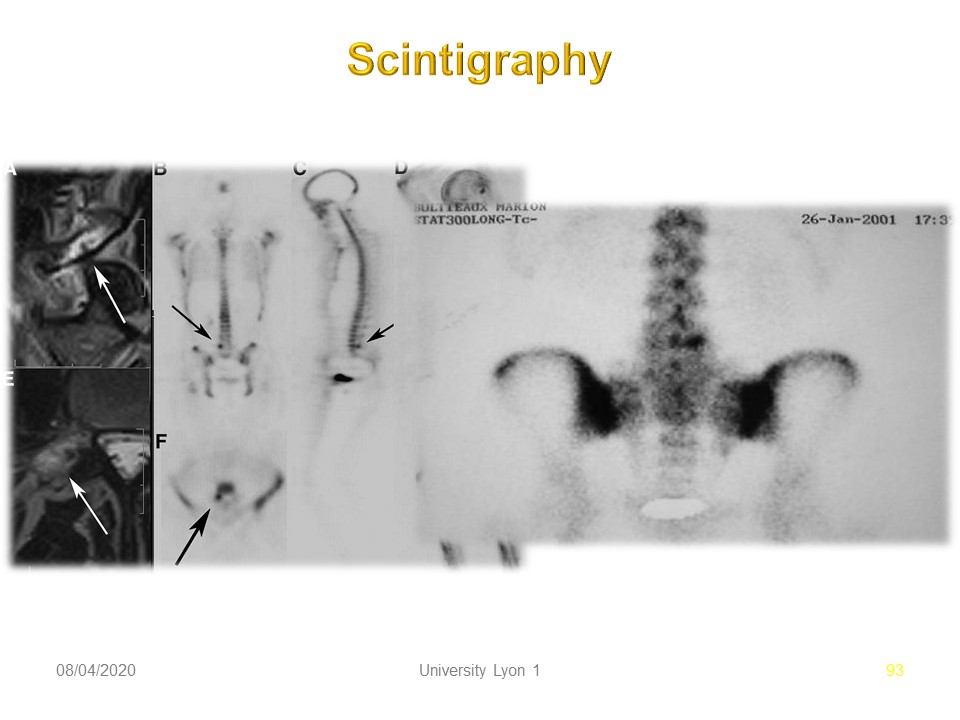 |
In doubtful cases or after trauma, the scintigraphy shows a hyper fixation, here at the level of the isthmus of L4. A positive scintigraphy justifies conservative orthopedic treatment.
|
 |
Here the technetium 99m technique demonstrates bilateral lysis. Technetium-99m - remains for 6 hours, allowing time in a hospital to isolate it, inject it to a patient as a radioactive marker to proceed, for example, to a bone scintigraphy. It emits a gamma photon without associated beta radiation.
|
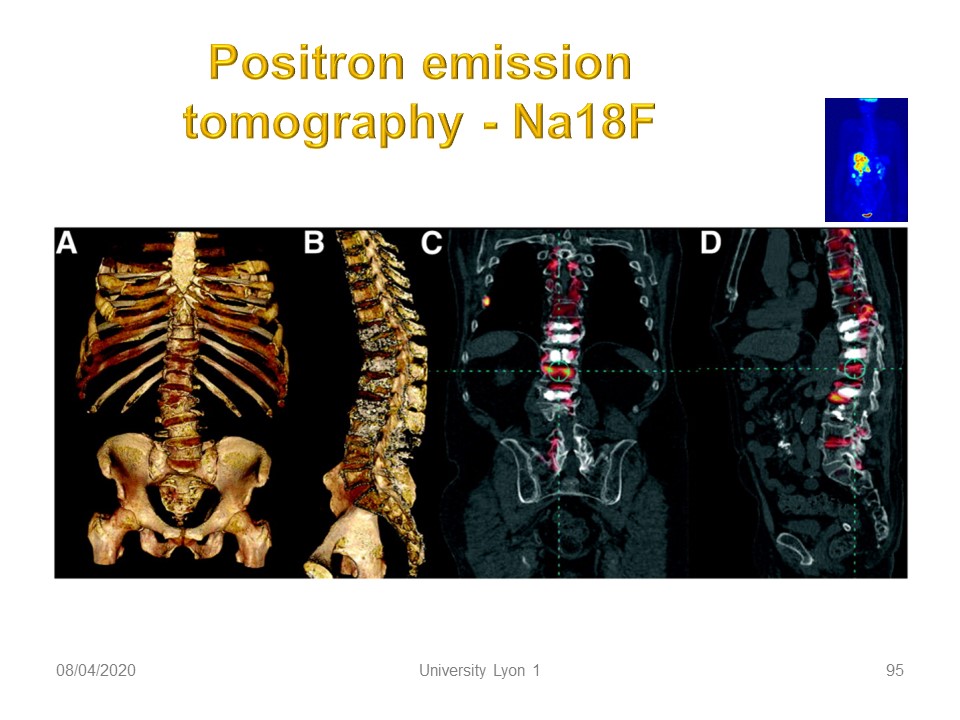 |
Sodium 18 fluoride positron emission tomography (PET) can also be used when bone metastases are suspected in adults.
|
 |
Here, evidence of isolated spondylolysis.
|
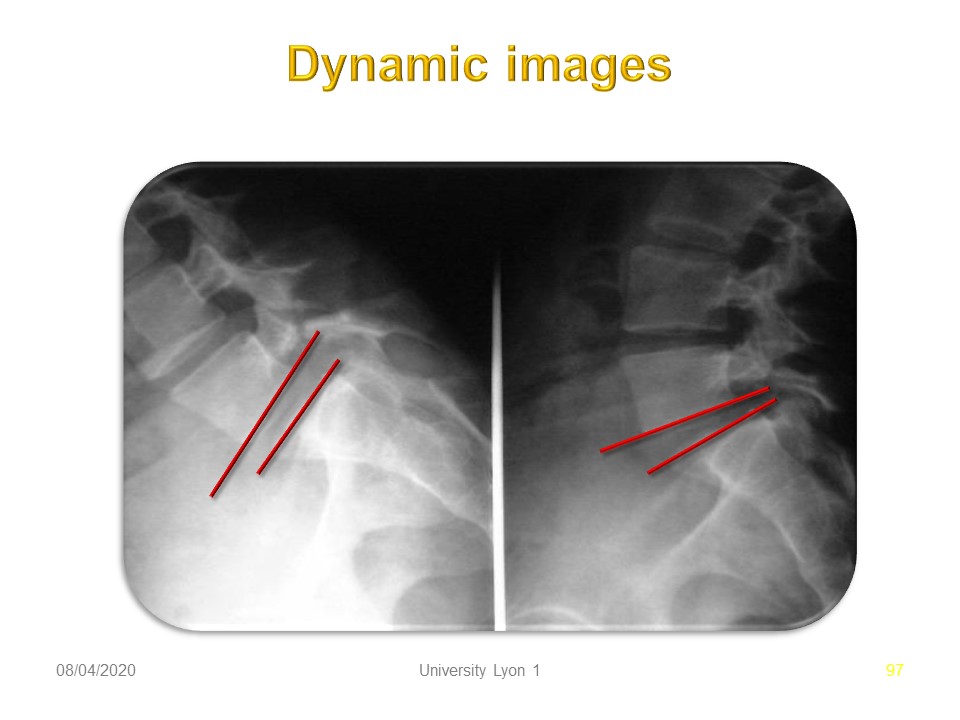 |
Painful instability is rare and can be highlighted by dynamic profile X-rays. Facet Joint laxity can change the range of motion. Here, there is little amplitude and harmonious passage from the anterior opening to the posterior opening.
|
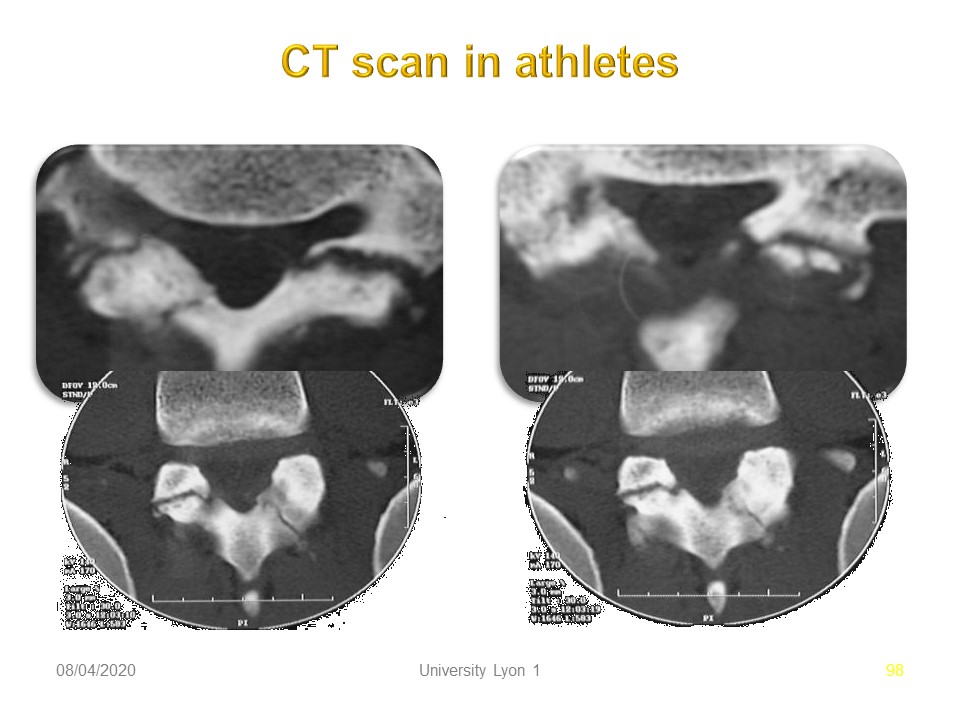 |
Same patient with horizontal scanner planes at different levels showing the important reconstruction effort. 1. Pars stress fracture. 2. Leave healed fracture. 3. Pars acute fracture.
|
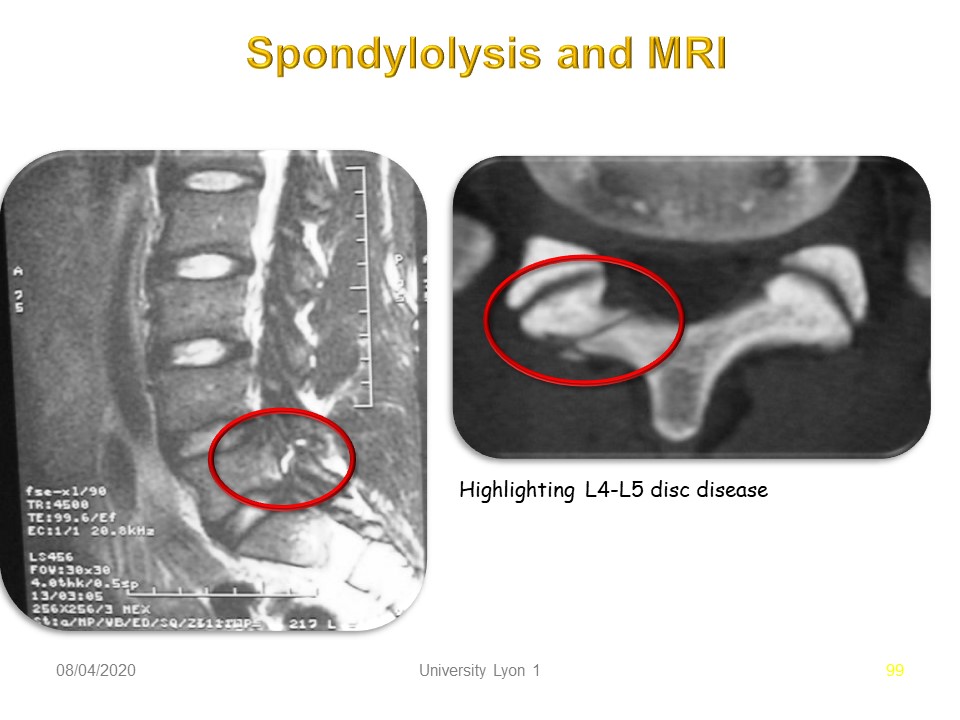 |
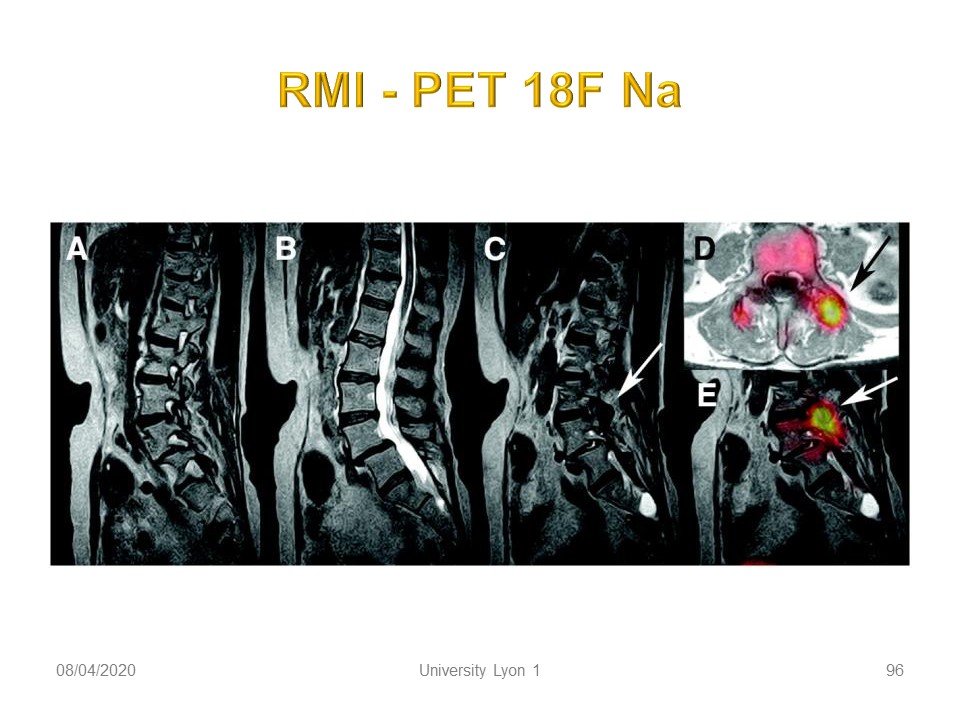
Magnetic Resonance Imaging shows above all, the hydration of the intervertebral disks, the appearance of the lysis on the transversal plane and possibly the quality of the paravertebral musculature.
|
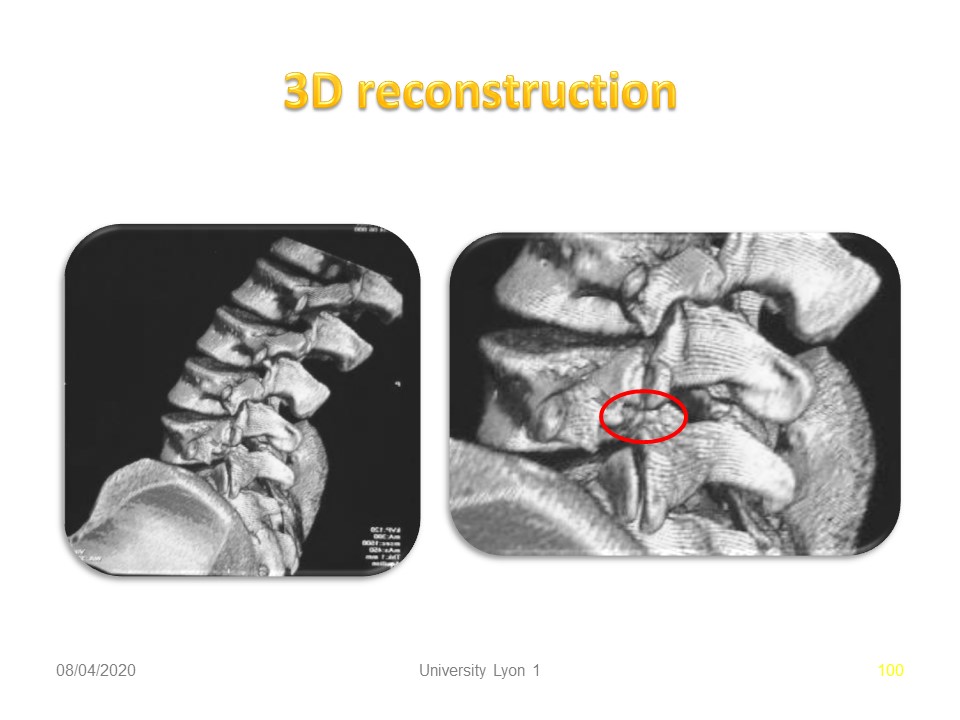 |
3D reconstruction by CT scan is very irradiant. It may be useful for highlighting an associated congenital malformation.
|
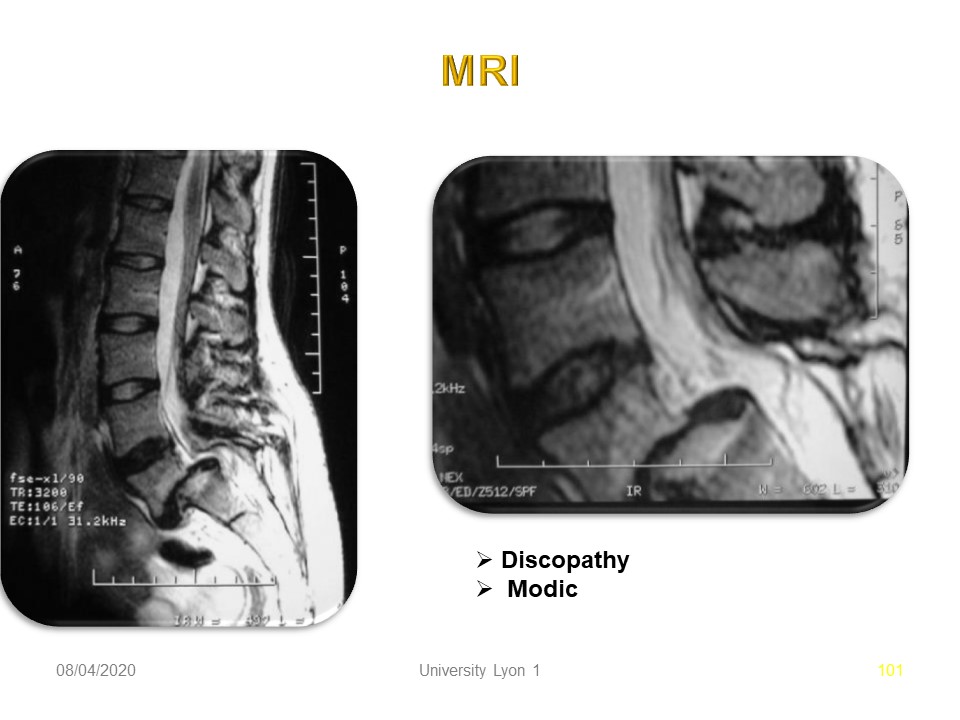 |
On the other hand, the MRI is not irradiating and puts in good effect the hydration of the disks. This is the complementary indication of choice in the context of spondylolisthesis. Here the discopathy L5-S1 is major with Modic sign.
|
 |
|
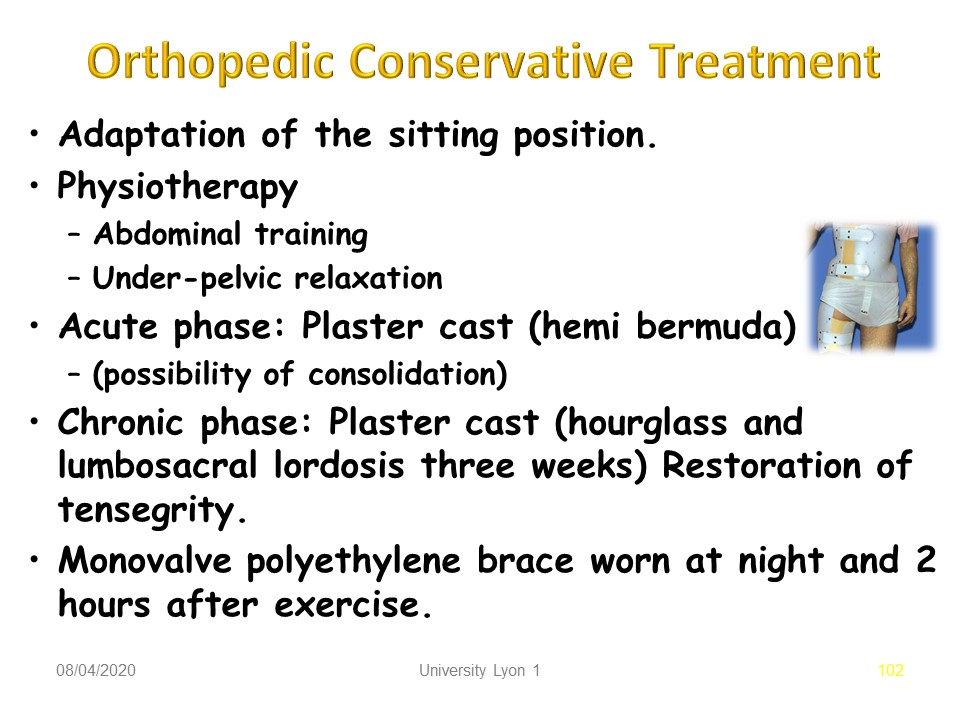 |
The conservative orthopedic treatment will be adapted. we distinguish: 1. Adaptation of the sitting position. 2. Physiotherapy with Abdominal strengthening and Under-pelvic relaxation. 2. In Acute phase: Plaster cast (hemi Bermuda) with possibility of consolidation. 3. In Chronic phase: Plaster cast (hourglass and lumbosacral lordosis three weeks) for Restoration of tensegrity. Then Monovalve polyethylene brace worn at night and 2 hours after exercise.
|
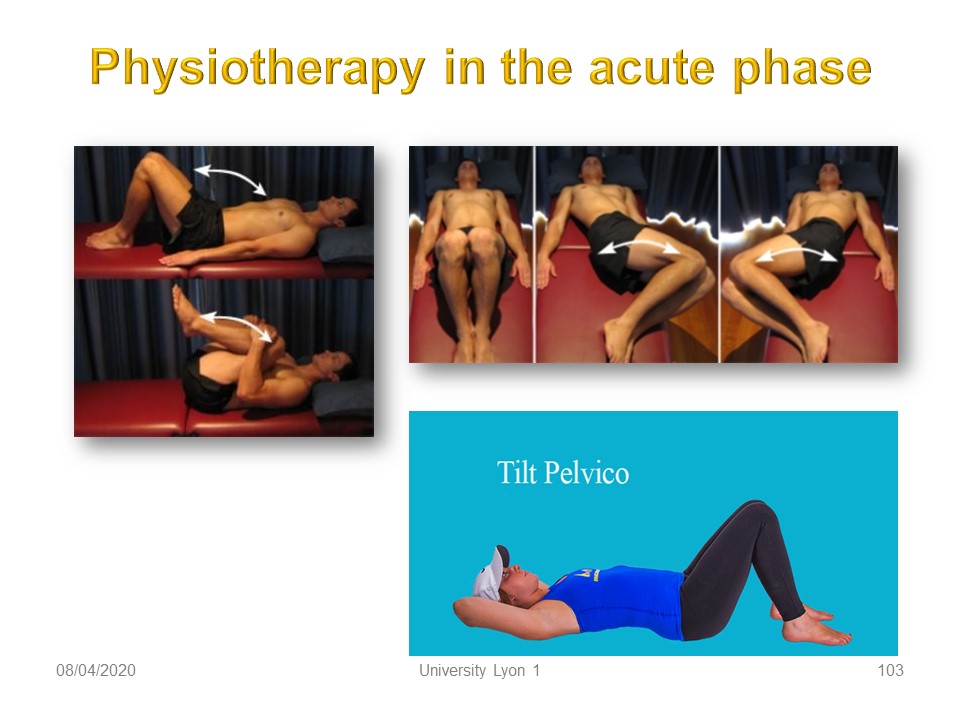 |
In the acute phase, physiotherapy is performed only in supine position. The goal is the gradual recovery of lumbosacral mobility. The movements are mainly in the sagittal plane. Static stretching on the left is obtained at the level of the posterior chains by a hyperflexion thighs and knees. The dynamic movements are limited to the pelvic tilt with alternation of lordosis and lumbar delordosis.
|
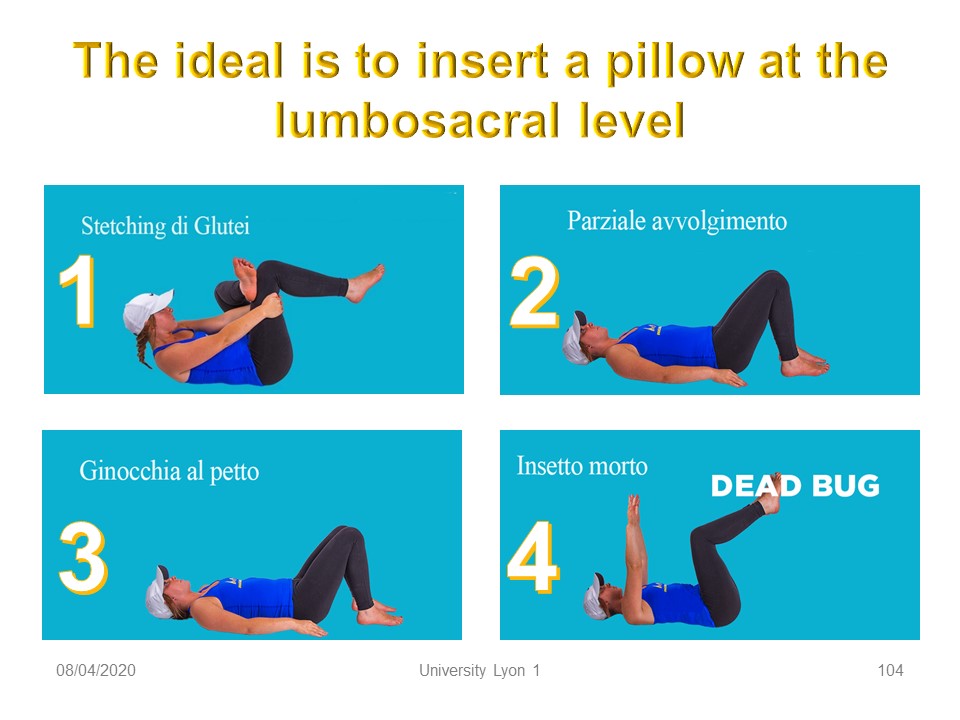 |
The most analgesic posture possible will be adapted using a lumbar cushion. Gradually, the muscular chains will be mobilized concentrically from the periphery to the lumbosacral junction and always in the sagittal plane. We will use: 1. the upper limbs in principle painless 2. the lower limbs respecting the rule of no pain. The progression is as follows: 1. stretching of the posterior chains. 2. Mobilization of the upper limbs. 3. Mobilization of the lower limbs. 4. beginning of dissociation of the belts.
|
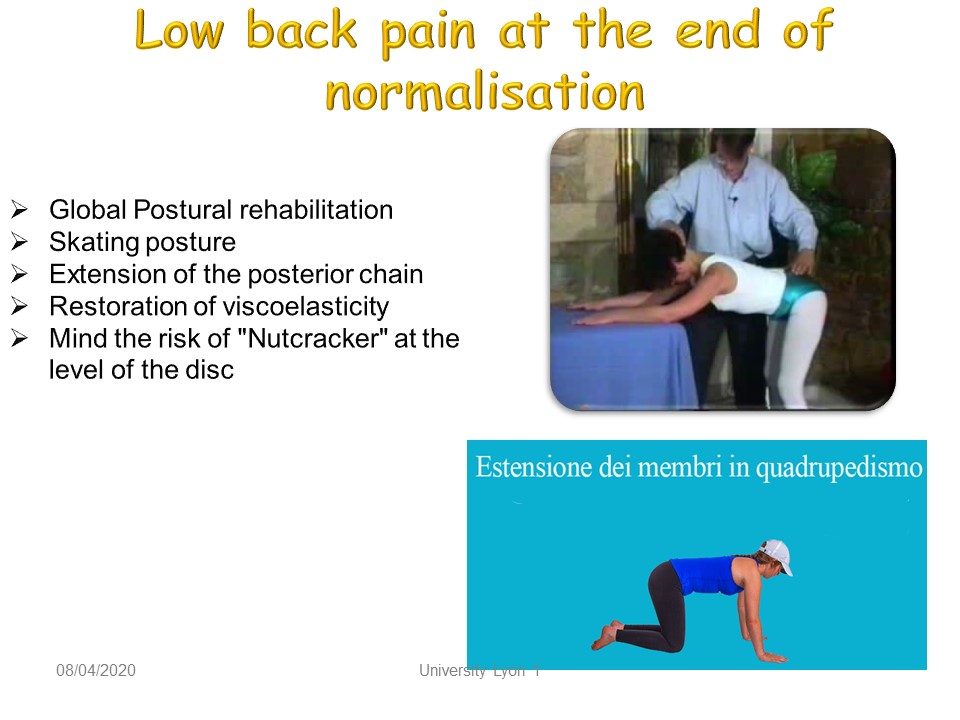 |
At the end of the acute phase, the exercises will be performed in closed kinetic chain, but with overall stress of the posterior and anterior chains. The rectitude of the lumbar spine will be maintained to limit the stress at the intervertebral disc. In the quadrupedy posture, the oblique chains will be trained by simultaneous extension of an upper limb and the contralateral lower limb.
|
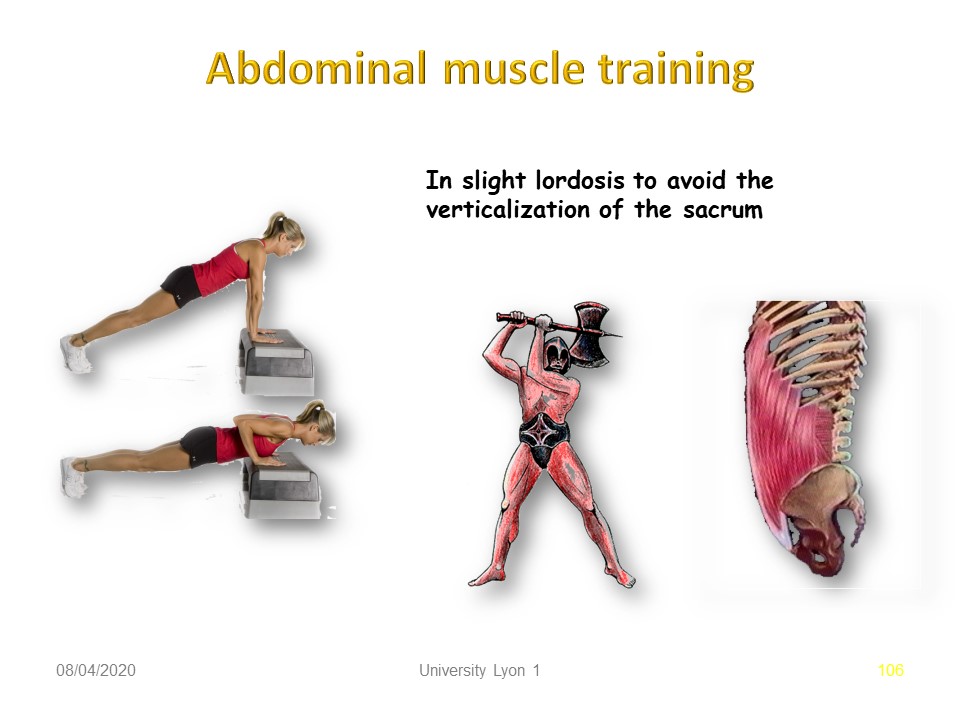 |
In the chronic phase, the abdominal and lumbar and pelvic musculature should be trained by cladding exercises.
|
 |
Whenever possible, plaster cast immobilization in the acute phase facilitates physiotherapy and above all allows the patient to remain active. According to the principles of the Lyon method, the objective is to readjust muscular tension at the lumbar-pelvic level (tensegrity). When there is an important analgesic attitude, the cast may be redone. Currently digital plaster can directly correct the antalgic posture on the computer.
|
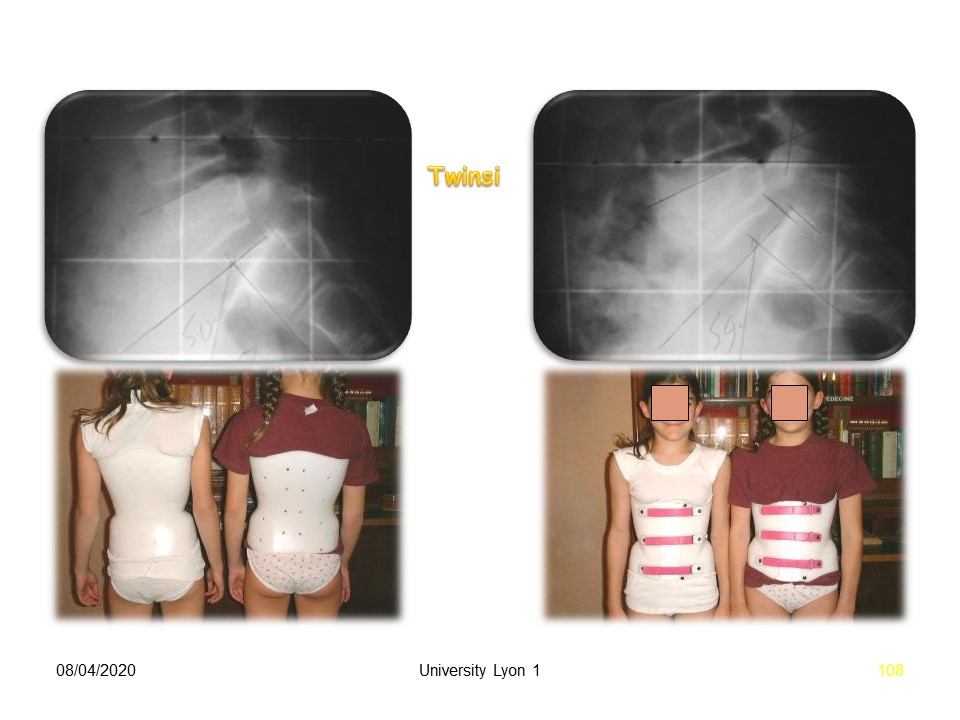 |
The brace used is a polyethylene in one piece, with anterior opening, as we see in these two twins. The two main objectives are: 1. mechanical discharge of the constraints by hourglass effect. 2. maintenance of lumbosacral lordosis to avoid verticalization of the sacrum. Currently the brace is made from beginning of the treatment with digital cast molding. The management is identical. 3 weeks of total time, then night-time and systematically for 2 hours after the sport.
|
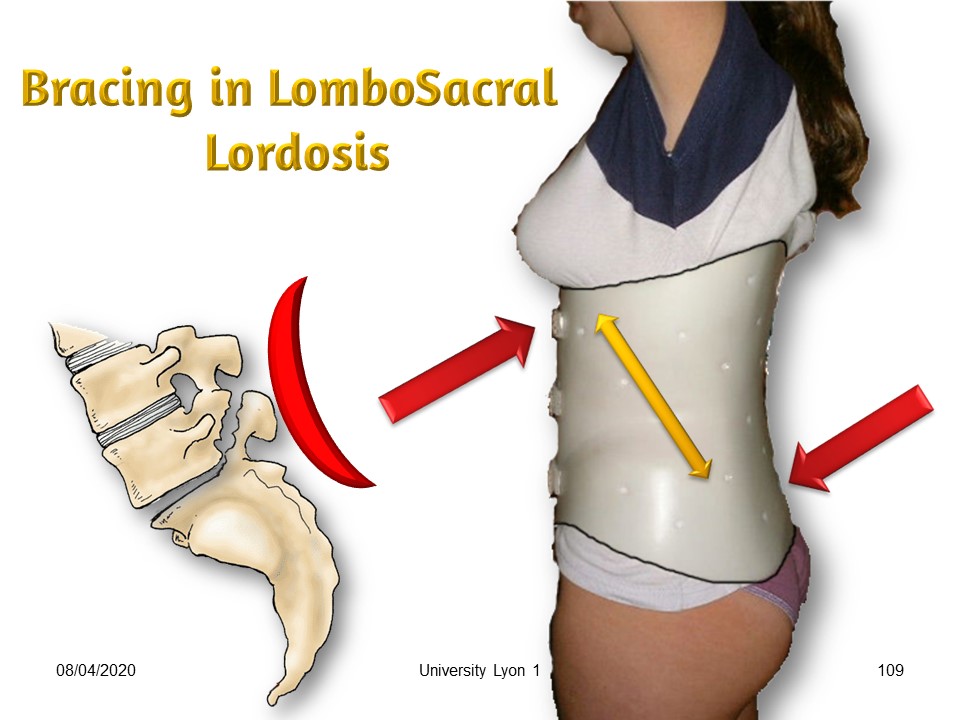 |
The difficulty is to locate the lordosis at the lumbosacral level. Lumbar hyperlordosis is usually seen with spondylolisthesis. The brace should not accentuate it. Therefore, lumbar lordosis will be corrected at its upper part by an extension sliding movement along the vertical axis at the false ribs level. Lumbosacral lordosis and elongation along the vertical axis will be performed simultaneously while maintaining the balance of the spine both in the frontal plane and in the sagittal plane.
|
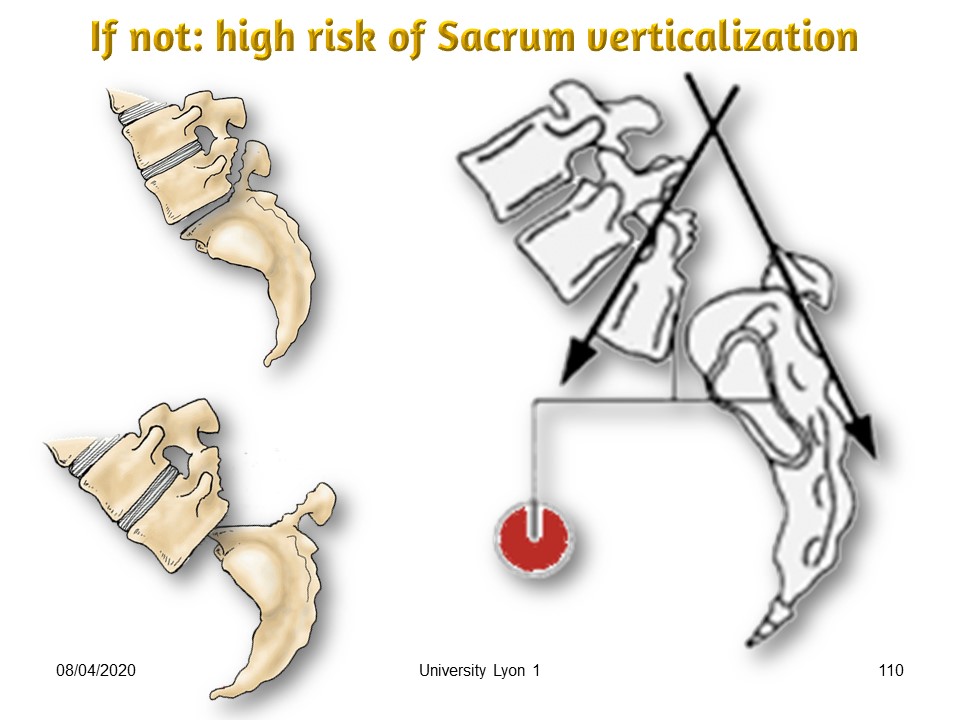 |
The brace should not facilitate the verticalization of the sacrum by a low posterior trim-line. In this case the lumbosacral angle decreases and there is an evolutive risk towards spondyloptosis. As soon as the lumbosacral angle is less than 110 °, the priority is lordosis.
|
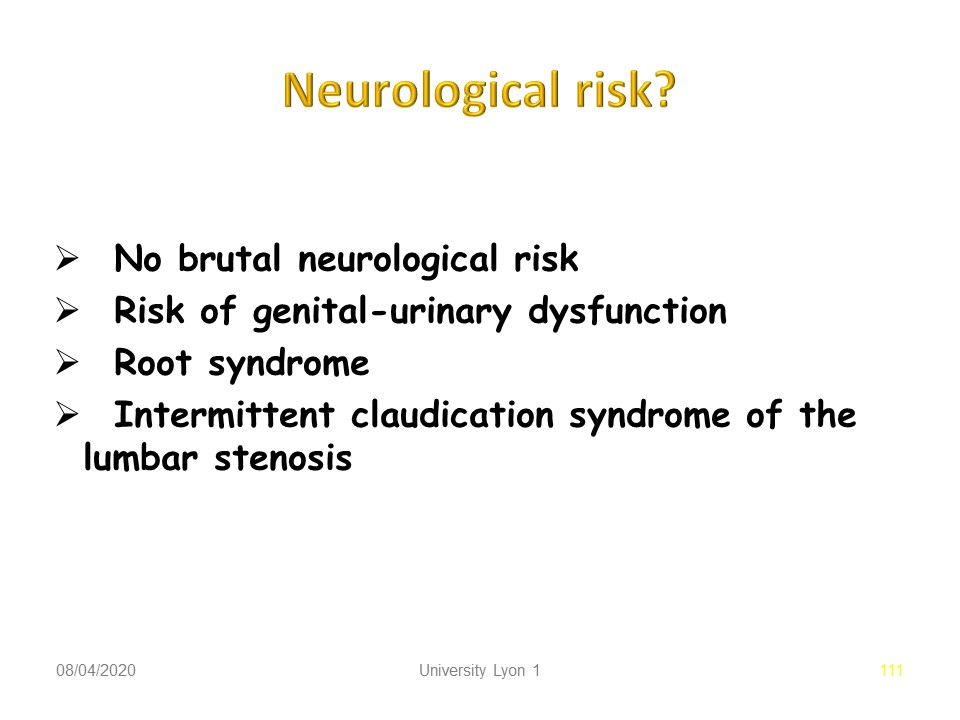 |
The neurological risk remains moderate in the spondylolisthesis of the child. Only rapidly slipping spondylolisthesis are accompanied by sciatica. On the other hand, the adult degenerative spondylolisthesis is painful. 3 mechanisms can irritate the nerves: 1. local inflammation; 2. Direct mechanical compression by an osteophyte for instance. 3. osteoarthritic stenosis with intermittent claudication.
|
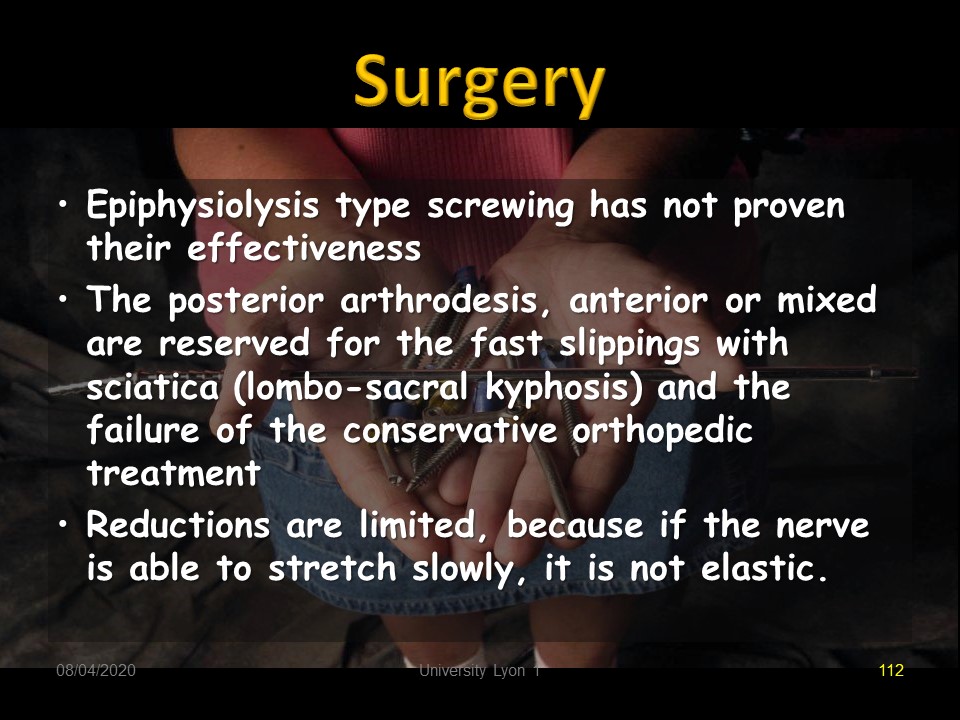 |
It is in these cases that surgery will be considered. For kids, epiphysiolysis type screwing has not proven their effectiveness. The posterior arthrodesis, anterior or mixed are reserved for the fast slipping with sciatica (lumbo-sacral kyphosis) and the failure of the conservative orthopedic treatment. Reductions are limited, because if the nerve can stretch slowly, it is not elastic.
|
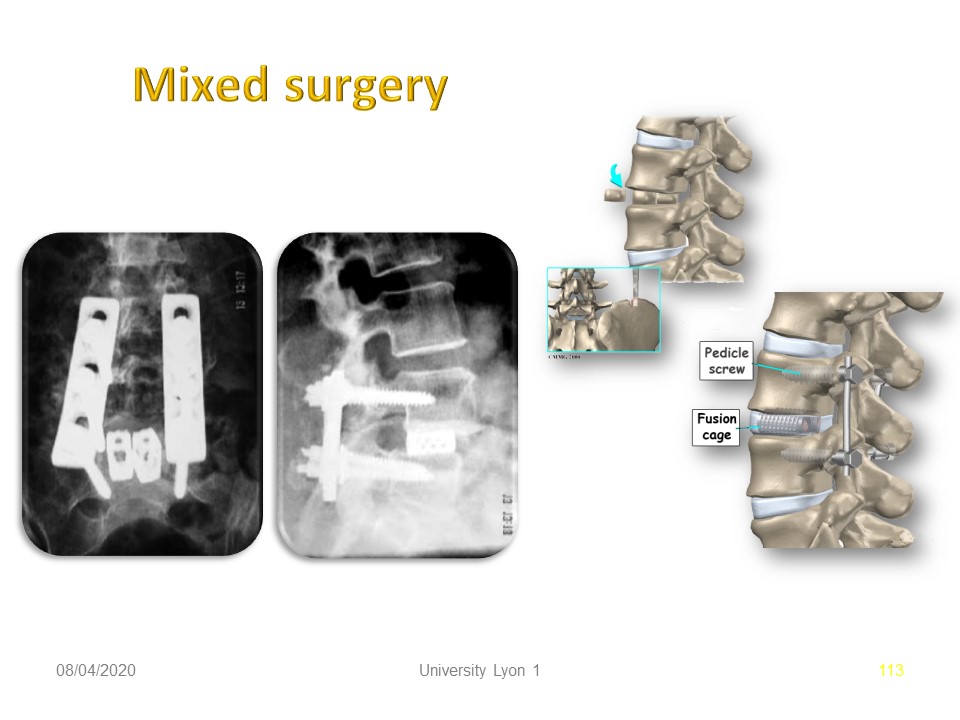 |
One of the ways to avoid the change in nerve length is to maintain the height between the two vertebral bodies by an anterior cage.
|
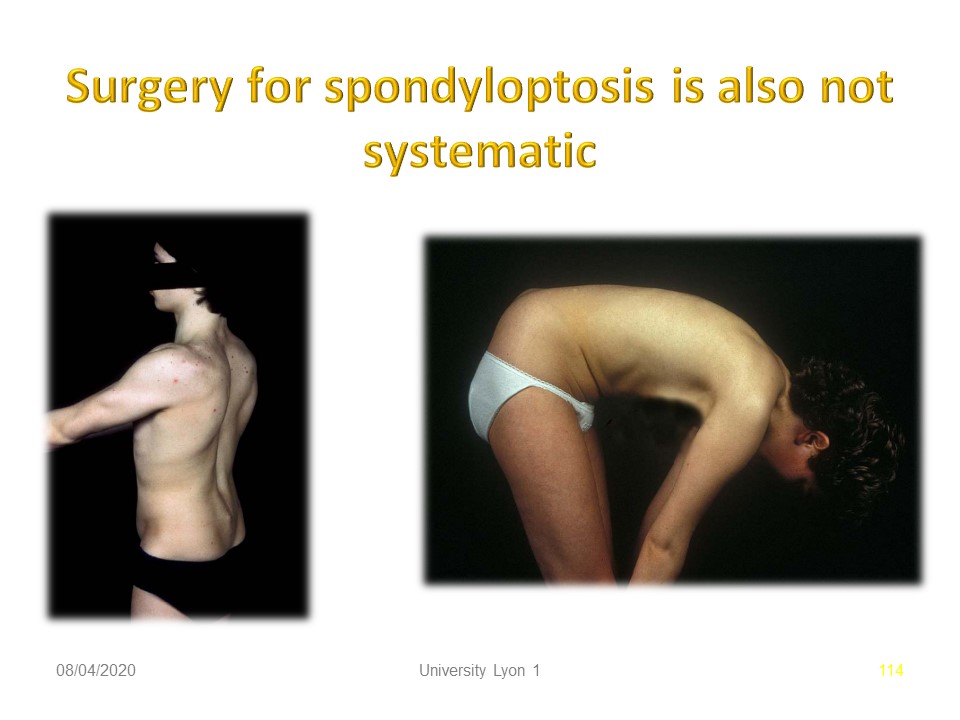 |
The clinical state is essential in the indication. Some spondyloptosis can be painless with limited functional impact and stable. In this case, there is no urgency for surgery.
|
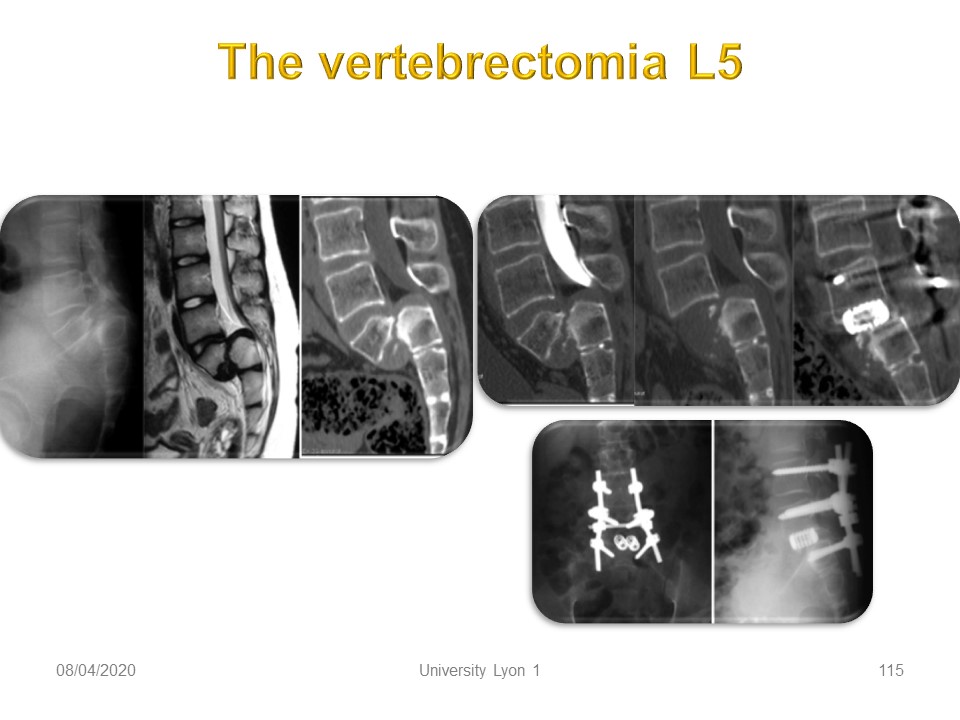 |
L5 vertebrectomy with double anterior and posterior arthrodesis can be an elegant solution at the orthopedic and neurosurgical level. However, It remains controversial.
|
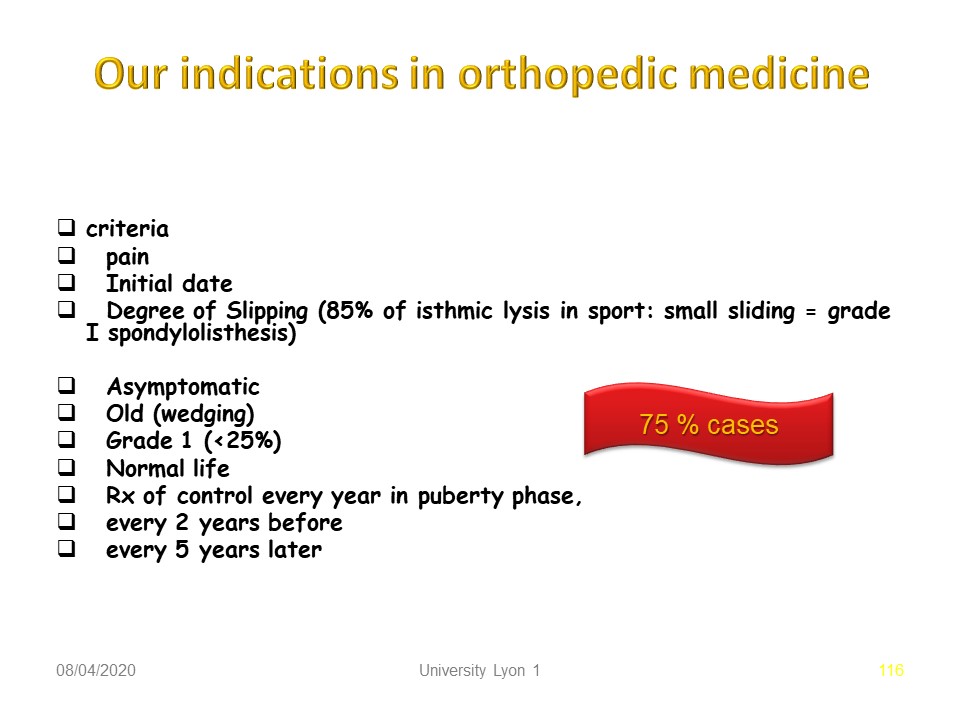 |
The indications for non-surgical orthopaedic treatment during the growth period are first of all clinical with the existence of pain on exercise reflecting instability. The importance of radiological slippage, a high lumbo-pelvic incidence or lumbo-sacral kyphosis below 110° are the most frequent indications, bearing in mind that for 3 out of 4 patients, observation and initial physiotherapy will be sufficient.
|
 |
The desire to continue sporting activity painlessly and safely should be discussed.
|
 |
|
 |
The majority of sportsmen and women prefer the pursuit of sport under the protection of the brace.
|
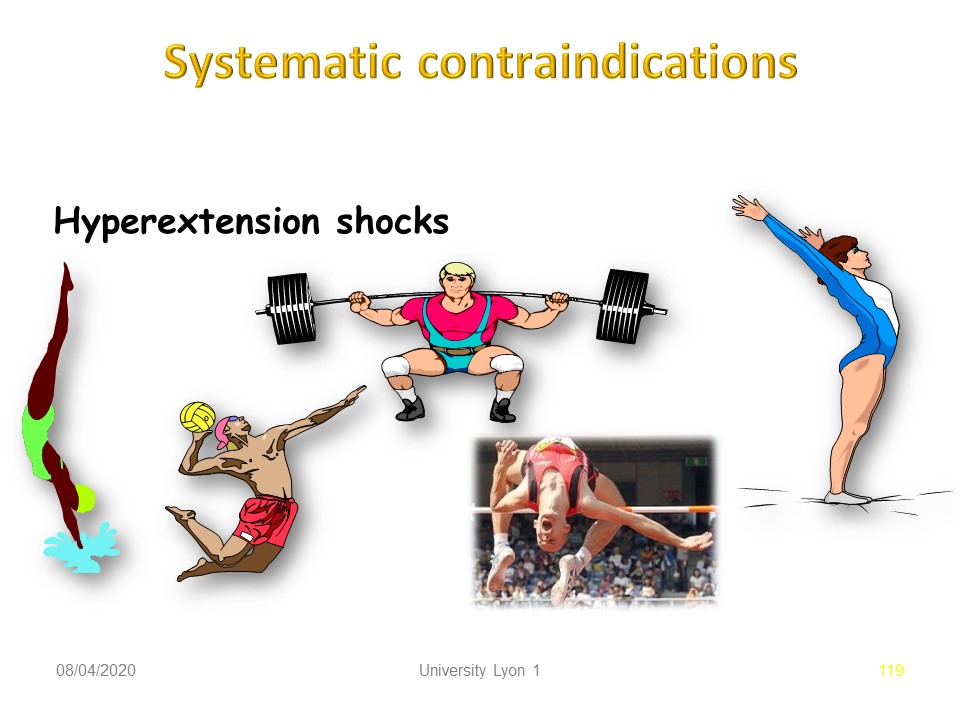 |
However, it is necessary to consider the type of sport practiced and to avoid all shocks in hyper-extension.
|
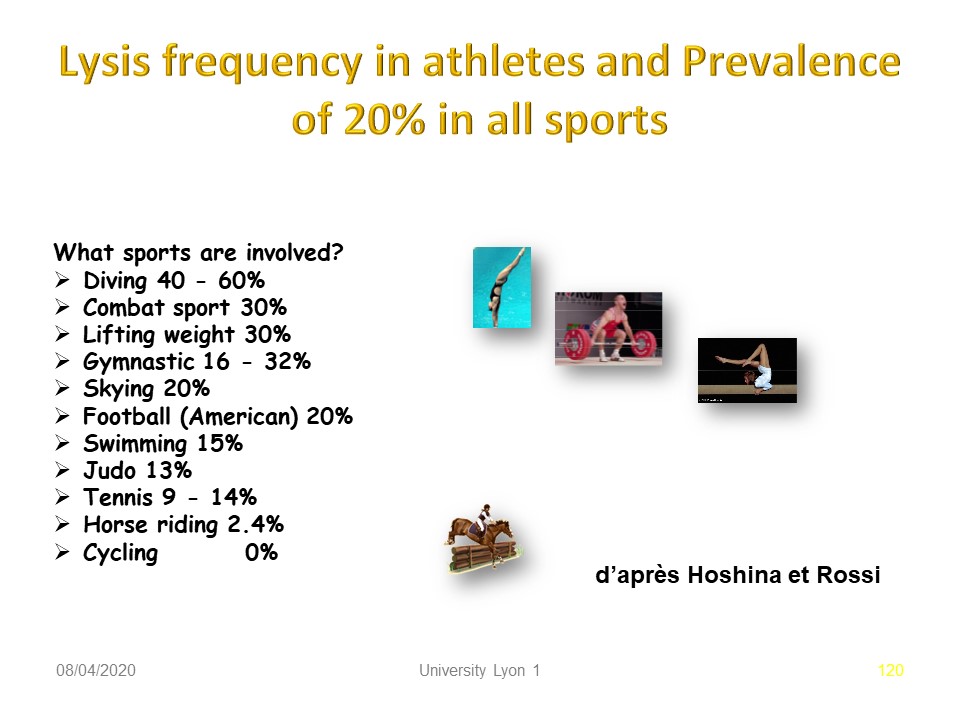 |
It is mostly in these sports that we find the highest frequency of spondylolysis. It should be noted that the frequency of spondylolysis during horse riding and cycling is lower than in the general population.
|
 |
|
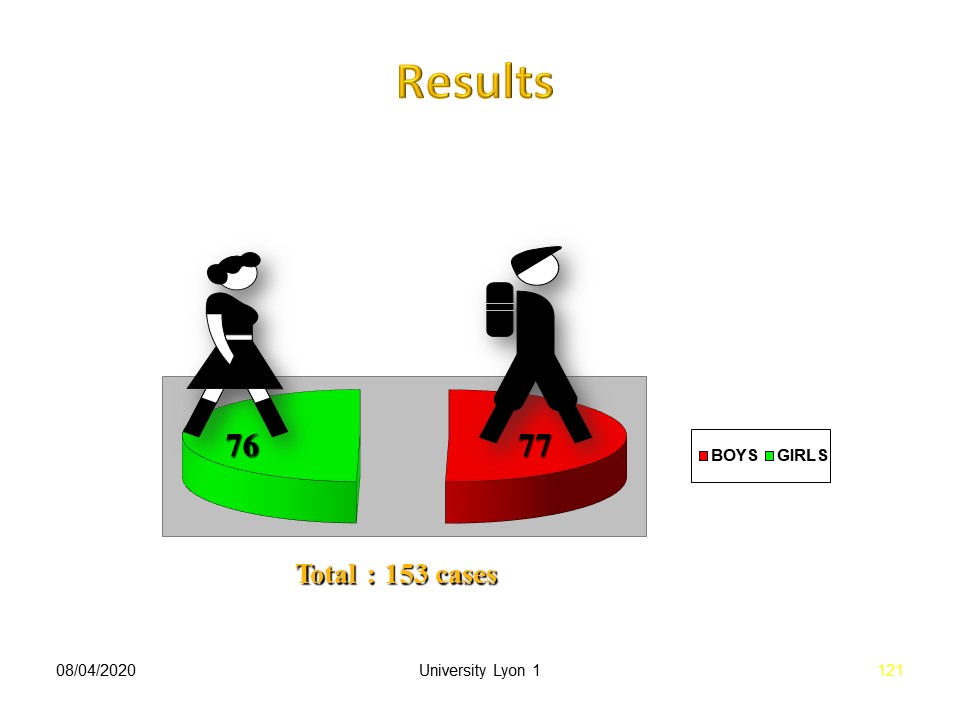 |
In our experience, we have treated as many girls as boys.
|
 |
The circumstances in which spondylolysis is discovered vary widely. Pain in extension is the most characteristic. It should be noted that lumbar spondylolysis never exists at birth, so it is not a congenital malformation.
|
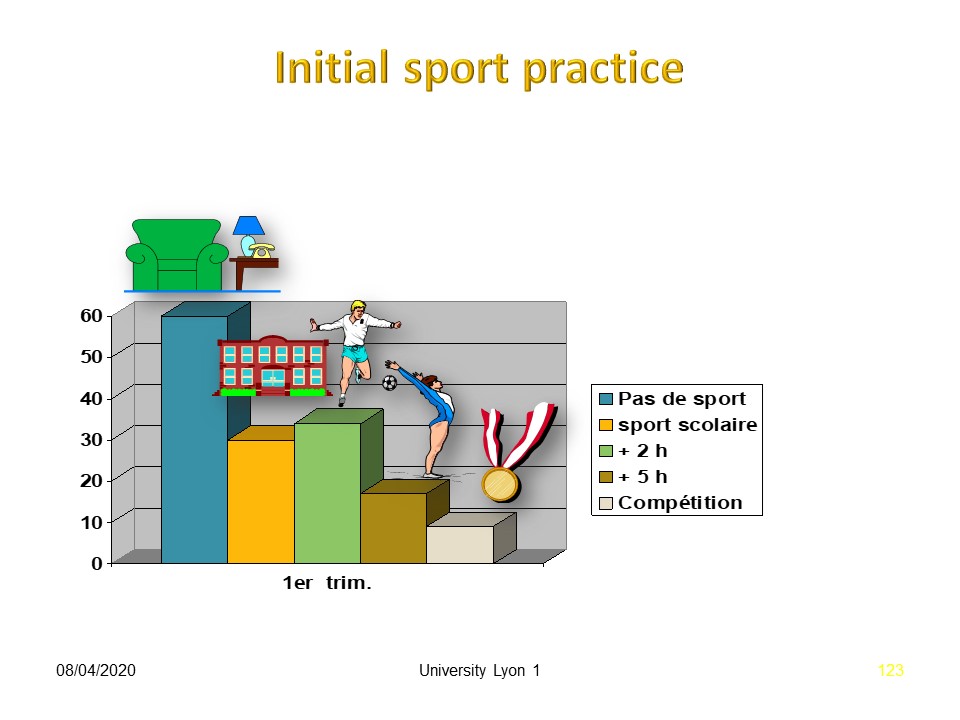 |
However, the majority of treated patients do not practice sports.
|
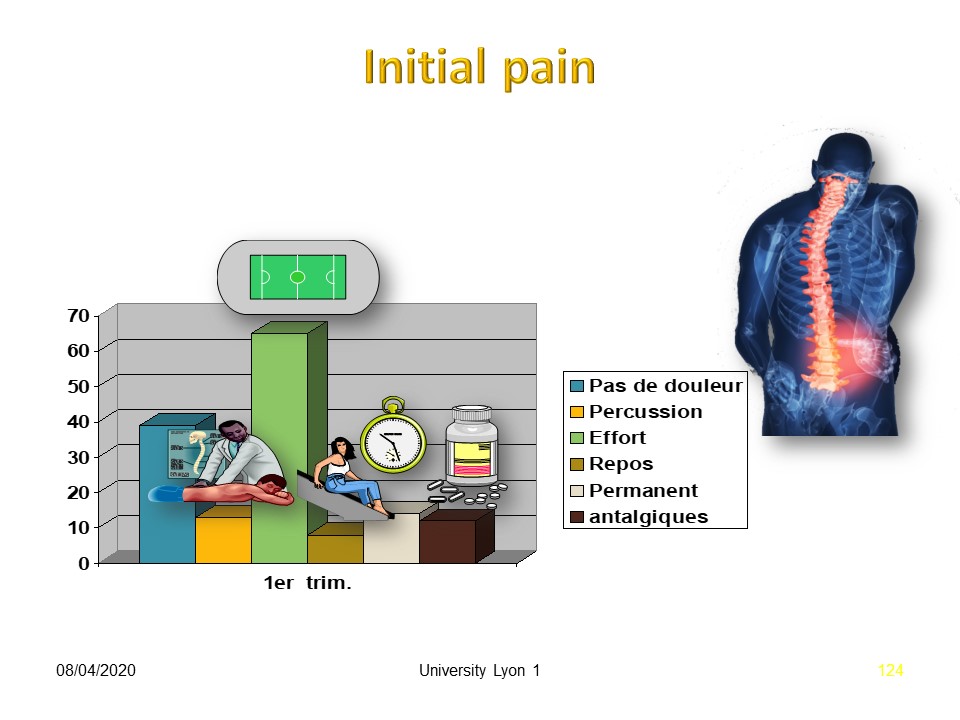 |
The majority of patients experience pain on efforts.
|
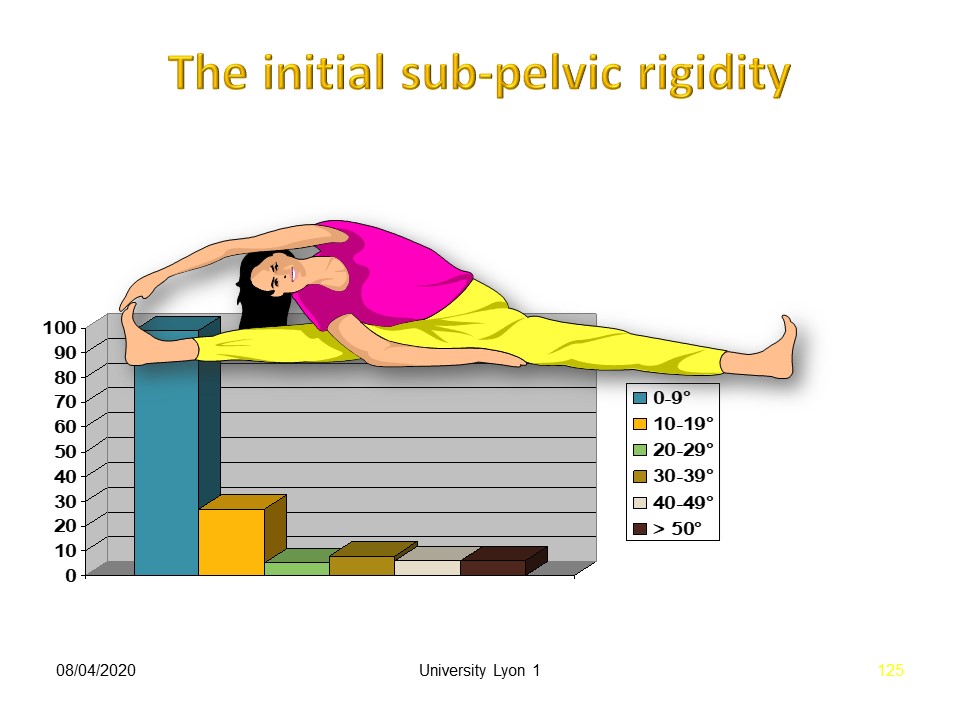 |
There is no sub-pelvic stiffness on clinical examination.
|
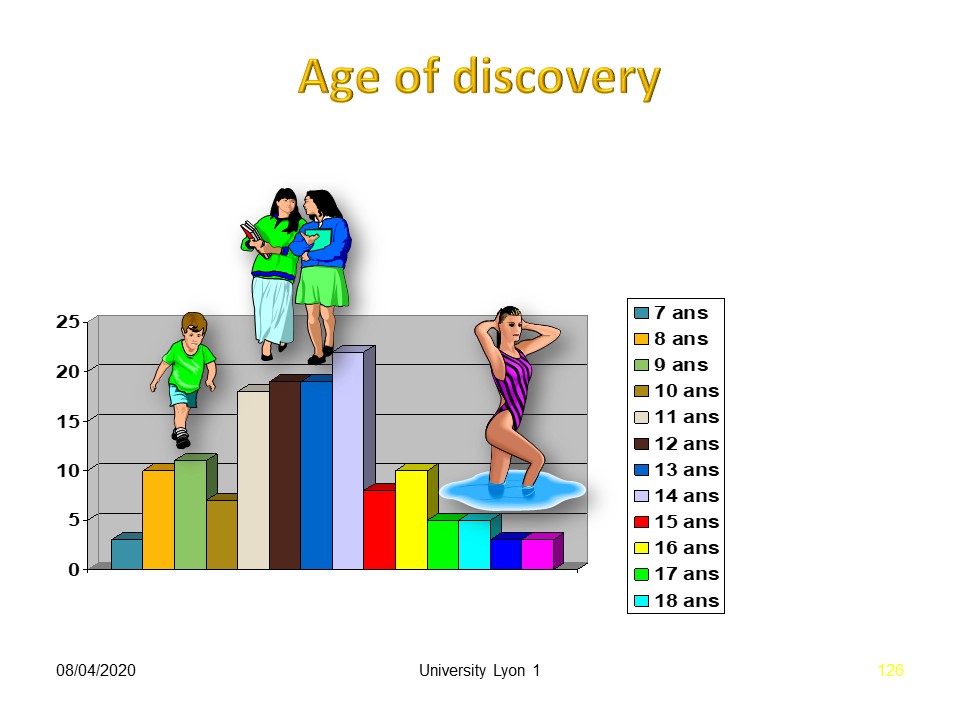 |
As with all vertebral deviations, the majority of patients are treated between 11 and 14 years of age.
|
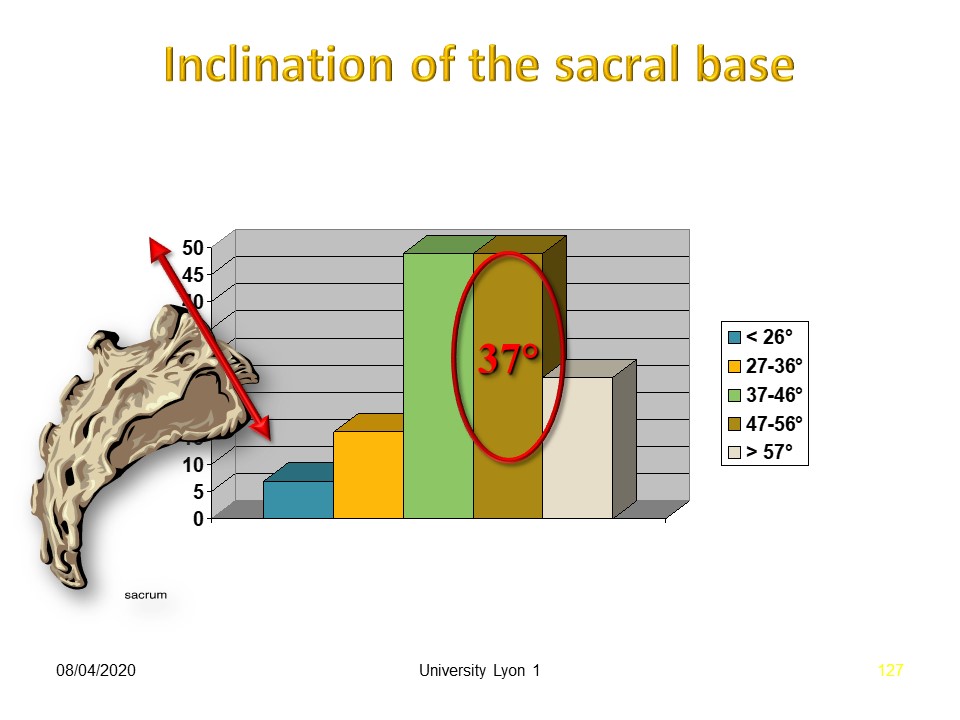 |
The vast majority of patients present with basic physiological sacral slope angulation. The dynamic micro-traumatic factor is probably more important than the morphostatic factor.
|
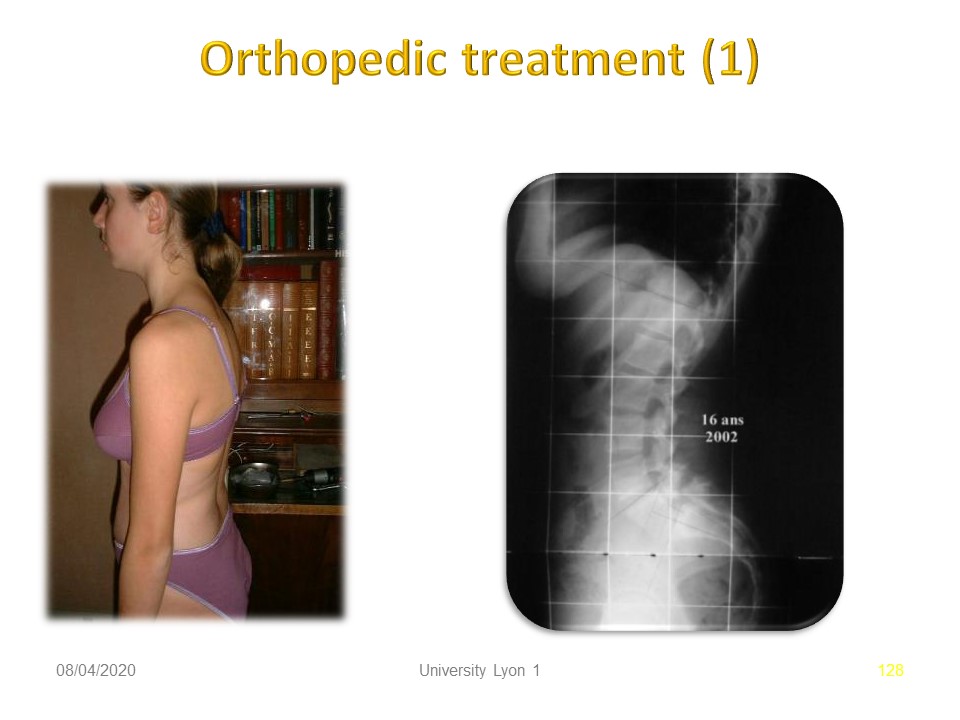 |
This hyperlordotic patient was treated at the age of 16 due to painful instability.
|
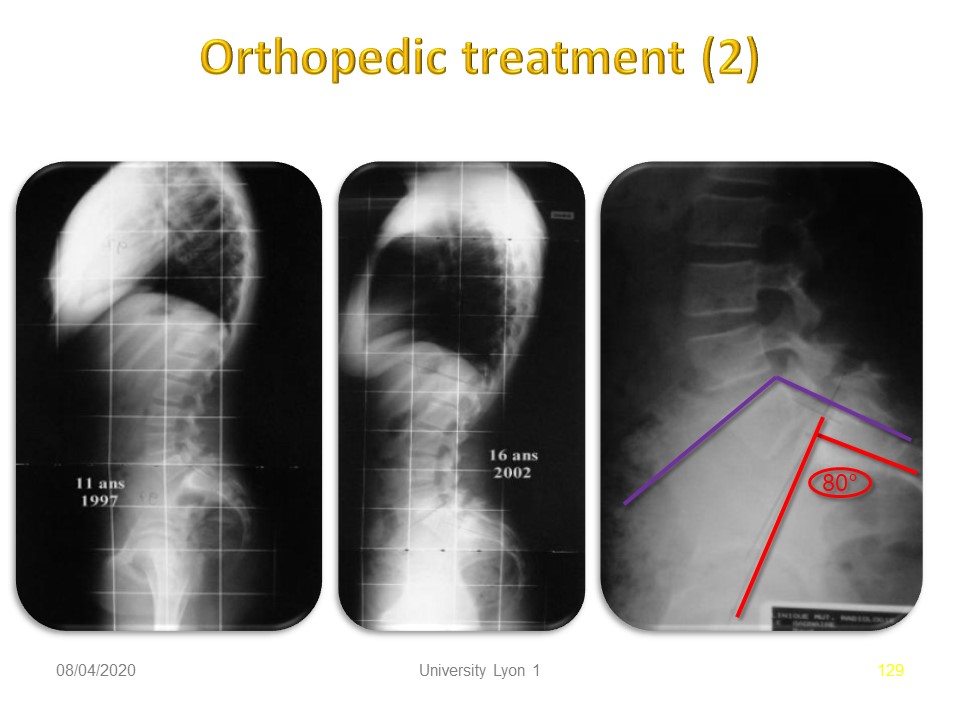 |
The radiological situation remained stable between the ages of 11 and 16, despite a high lumbo-pelvic incidence which explains the current pain.
|
 |
The brace was made in lumbo-sacral lordosis and correction of upper lumbar lordosis. The brace is worn 24 hours a day for 3 weeks and then for 4 hours every day especially after sports activity for a minimum of 6 months.
|
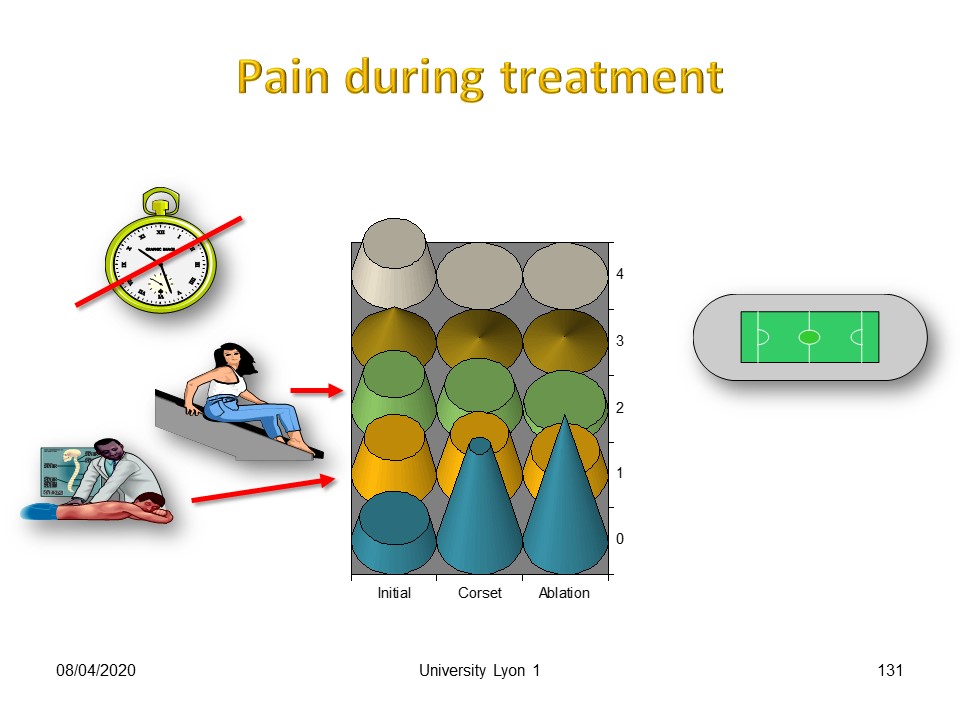 |
Results on pain are usually very fast.
|
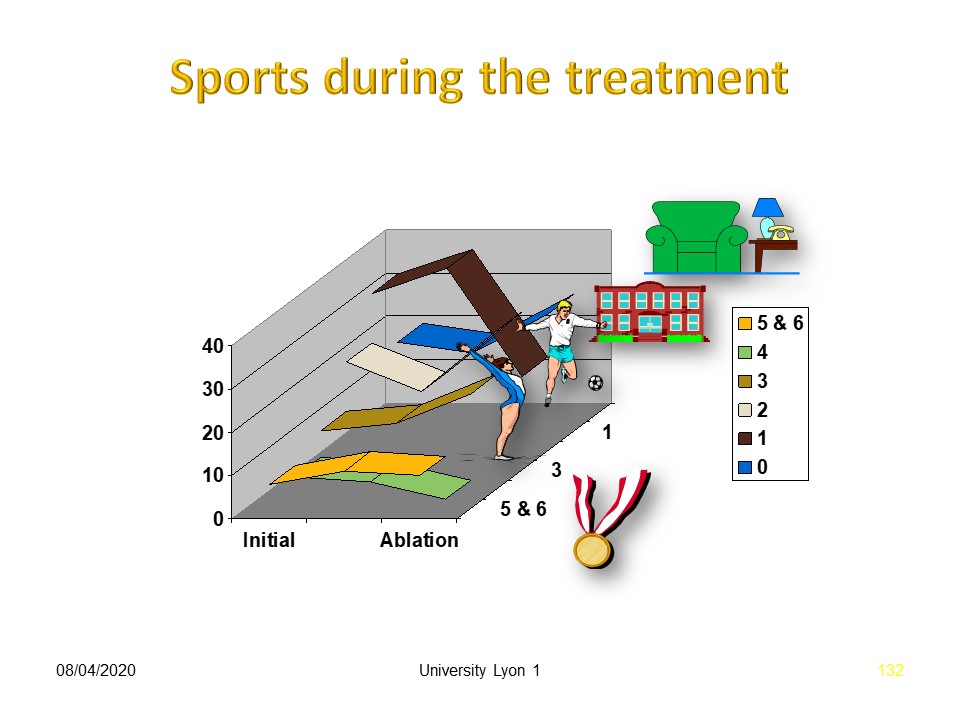 |
Sporting activity is continued and even increased in the majority of cases, compared to the initial situation.
|
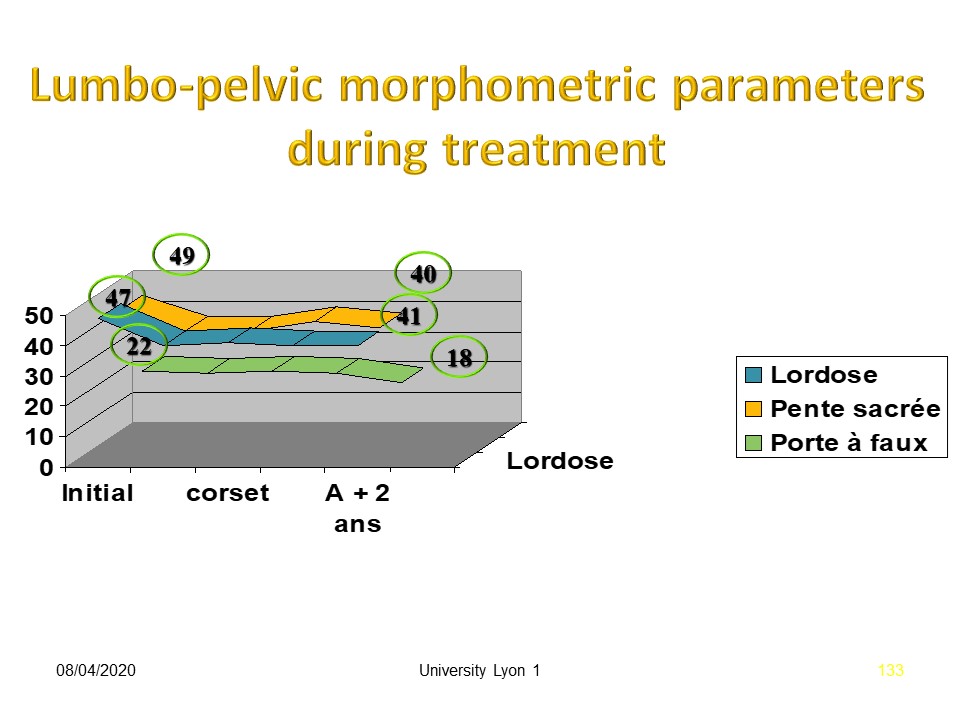 |
Morphostatic parameters are very slightly improved during treatment.
|
 |
Consolidation is possible, especially in cases of acute spondylolysis with early treatment. If patients are seen later, consolidation occurs in 10% of cases.
|
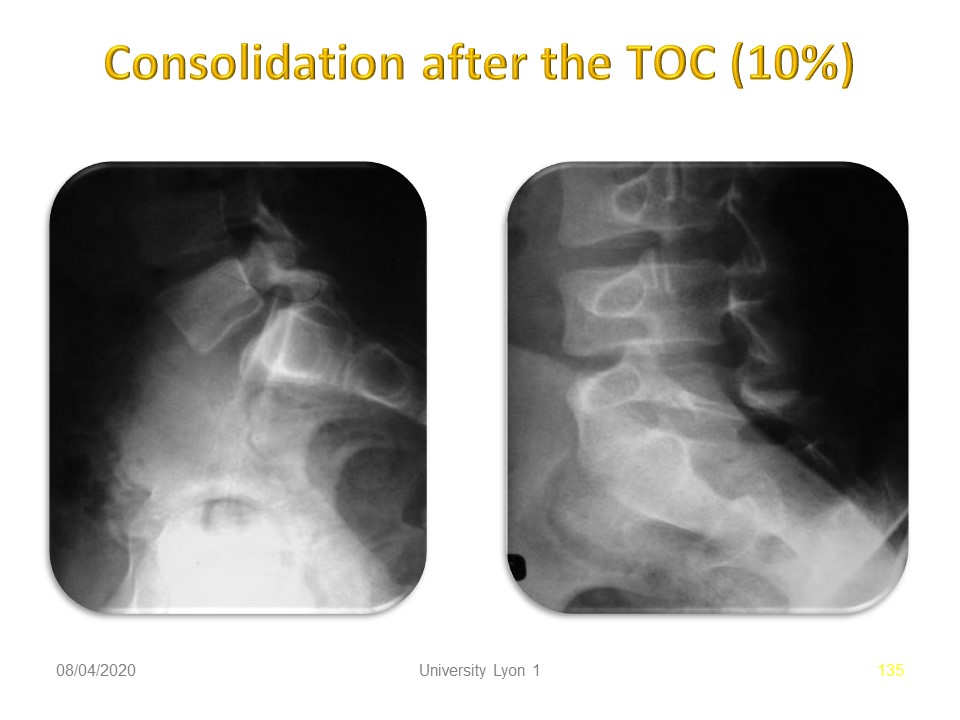 |
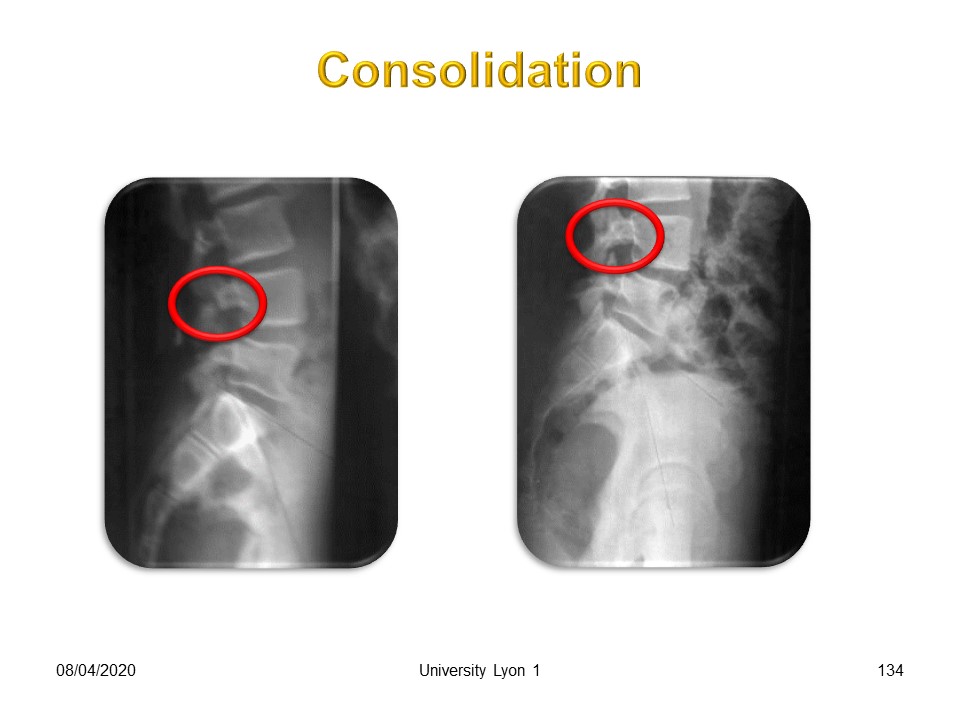
Here is an example of consolidation with isthmus lengthening.
|
 |
The publications show results that are more or less identical to our experience with pain relief and return to sport within 2 months.
|
 |
In conclusion, non-surgical orthopaedic treatment is an excellent solution for athletes with increased orthopaedic safety.
|
 |
This treatment remains poorly known and most doctors still advise against continuing sports activities and forcing the child to be sedentary.
|
 |
|
 |
Given the frequency of spondylolysis, this is a public health problem. Non-surgical orthopaedic treatment should be used much more as long as the brace is made correctly in lumbo-sacral lordosis to avoid verticalization of the sacrum.
|
 |

To register for Certification, please contact SSOL

|